Compare Movfor (Molnupiravir) with Other COVID-19 Antiviral Treatments
 Oct, 29 2025
Oct, 29 2025
Antiviral Treatment Advisor
Personalized COVID-19 Antiviral Advisor
Answer a few questions to find out which antiviral treatment might be most appropriate for your situation based on clinical guidelines.
Your Health Information
Treatment Recommendations
Results will appear here
Enter your information above and click "Get Recommendations" to see which antiviral treatment might be appropriate for you.
Paxlovid (Nirmatrelvir + Ritonavir)
RecommendedEffectiveness: Reduces hospitalization risk by ~89% when taken early
Recommended if: You're over 60, have chronic conditions, and don't take medications that interact with Paxlovid.
Not recommended if: You're taking blood thinners, statins, or certain heart/mental health medications.
Movfor (Molnupiravir)
AlternativeEffectiveness: Reduces hospitalization risk by ~30% when taken early
Recommended if: You're taking medications that interact with Paxlovid, or if Paxlovid is unavailable.
Not recommended if: You're pregnant, breastfeeding, or under 18.
Remdesivir
AlternativeEffectiveness: Reduces hospital stay by ~30% and lowers death risk
Recommended if: You can't take oral medications or both Paxlovid and Molnupiravir are contraindicated.
Not recommended if: You're able to take oral medications.
No Antiviral Recommended
No treatmentRecommendation: No antiviral treatment is recommended based on your current situation.
Reason: Antivirals are most effective when taken within 5 days of symptom onset, and you're not at high risk for severe disease. Rest, hydration, and standard care may be sufficient.
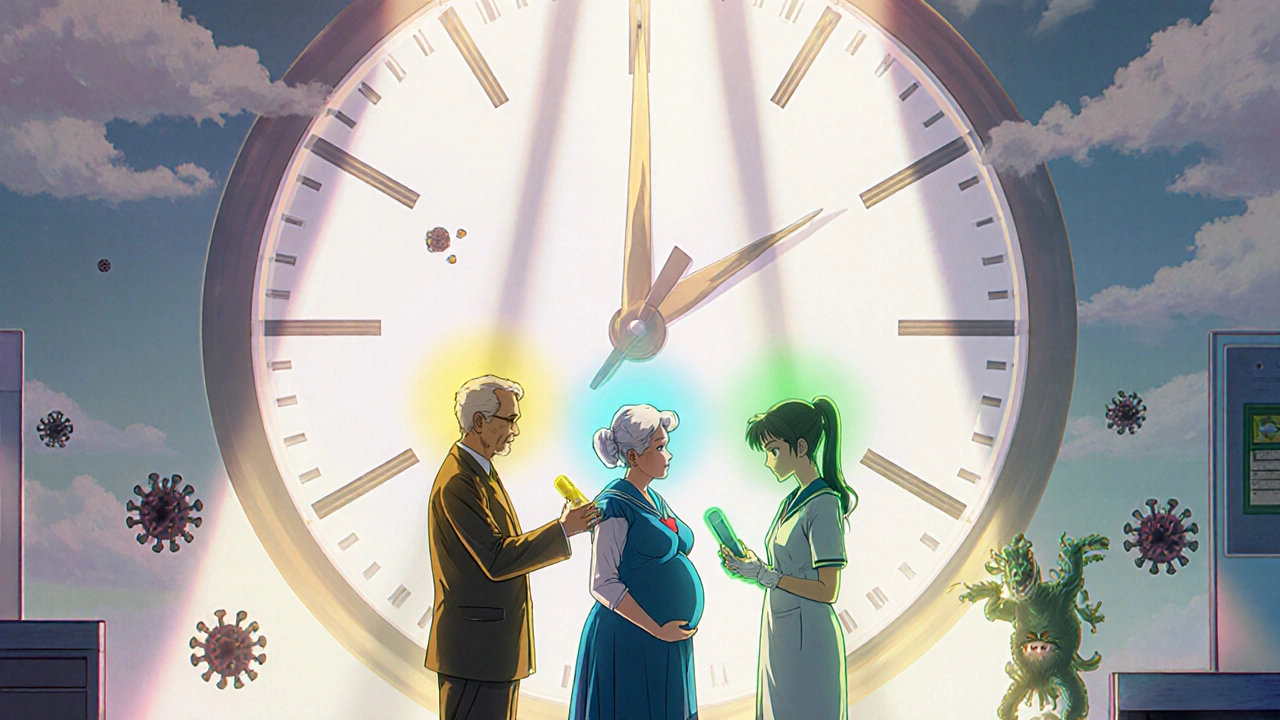
When you’re told you have COVID-19 and are at risk for severe illness, your doctor might mention Movfor - the brand name for molnupiravir. But you’ve probably heard of other options too, like Paxlovid. So which one actually works better? And does it even matter? The truth is, not all antivirals are created equal. Some work faster. Some have fewer side effects. Some are easier to take. And some aren’t even available in every country.
What is Movfor (Molnupiravir)?
Movfor is the brand name for molnupiravir, an oral antiviral medication designed to stop the SARS-CoV-2 virus from replicating in the body. It was first authorized for emergency use in late 2021 and is approved in over 40 countries, including New Zealand, the UK, and Australia.
It comes as a capsule you take twice a day for five days. You start it as soon as possible after symptoms begin - ideally within five days. The goal isn’t to cure you overnight. It’s to reduce the chance you’ll end up in the hospital. Clinical trials showed it cut hospitalizations by about 30% in high-risk adults. That’s not perfect, but it’s something.
How it works is unique. Molnupiravir tricks the virus into making copying errors as it tries to reproduce. Think of it like giving the virus a faulty blueprint. Eventually, it builds so many broken copies that it can’t keep spreading. This mechanism is why it’s been studied for other RNA viruses too, like influenza and Ebola.
Paxlovid: The Current Gold Standard
If you’ve been following COVID-19 treatments, you’ve likely heard of Paxlovid, a combination of nirmatrelvir and ritonavir, approved for high-risk patients with mild to moderate COVID-19.
Paxlovid is taken as three pills twice a day for five days. It’s more effective than molnupiravir - reducing hospitalizations by around 89% in clinical trials when taken early. That’s a huge difference. It’s also the most widely recommended antiviral in the U.S., the UK, and New Zealand for people over 60 or those with chronic conditions like diabetes or heart disease.
But Paxlovid has a catch: it interacts with a lot of common medications. If you’re on blood thinners, statins, or certain heart or mental health drugs, Paxlovid can be dangerous. Your pharmacist or doctor needs to check your full medication list before prescribing it. That’s why some people get molnupiravir instead - not because it’s better, but because it’s safer for their existing regimen.
Remdesivir: The IV Option
Not everyone can take pills. If you’re too sick to swallow or can’t manage oral meds at home, remdesivir, an intravenous antiviral given over three days in a clinic or hospital. It’s not a first-line choice for outpatient care, but it’s the only antiviral approved for use in hospitalized patients.
Remdesivir is also used off-label for high-risk outpatients who can’t take oral drugs. You get it via IV drip, usually over 60 minutes. That means you need to travel to a medical center. For people in rural areas or with mobility issues, that’s a big barrier. But it’s still a solid option when oral antivirals aren’t possible.
Studies show remdesivir reduces hospital stay length by about 30% and lowers death risk in early-stage patients. It’s not as convenient as pills, but it’s more potent. It’s also one of the few antivirals approved for children under 12.
Other Alternatives: What’s Out There?
Outside of these three, options are limited. In some countries, you might find:
- Ensitrelvir - approved in Japan and South Korea. It’s a newer pill taken once daily for five days. Early data suggests it’s as effective as Paxlovid with fewer drug interactions.
- Favipiravir - used in Russia and India. Less proven, with mixed trial results and higher side effect rates. Not recommended by WHO or CDC.
- Fluvoxamine - an antidepressant studied for COVID-19. Some small trials showed reduced hospitalizations, but it’s not approved for this use anywhere. Don’t self-medicate.
For most people in New Zealand, Australia, or the U.S., the real choices are Movfor, Paxlovid, or Remdesivir. Everything else is either unavailable, unproven, or not recommended.

Side Effects: Which One Is Easier to Tolerate?
Side effects matter. If you feel worse taking the medicine than you did with the virus, you might skip it. Here’s how they compare:
| Medication | Common Side Effects | Serious Risks |
|---|---|---|
| Movfor (Molnupiravir) | Nausea, diarrhea, headache | Potential DNA damage in animal studies; not recommended for pregnant people or those under 18 |
| Paxlovid | Altered taste, high blood pressure, muscle aches | Drug interactions - can be life-threatening with statins, blood thinners, or anti-seizure meds |
| Remdesivir | Nausea, elevated liver enzymes | Infusion reactions (rare), kidney stress in people with existing issues |
Movfor has the most concerning long-term safety flags. Animal studies showed it could cause mutations in DNA. That’s why it’s not given to pregnant people or anyone under 18. Paxlovid doesn’t carry that risk, but its drug interactions are a minefield. Remdesivir is safest in that regard - no known interactions - but you have to sit through an IV.
Who Gets Which Treatment?
There’s no one-size-fits-all. Your doctor picks based on your health, meds, age, and access.
- Paxlovid is first choice for healthy adults over 60 or with chronic illness - if your other meds don’t clash.
- Movfor is used when Paxlovid isn’t safe due to drug interactions, or if Paxlovid isn’t available.
- Remdesivir is for people who can’t take oral meds, or when both pills are contraindicated.
In New Zealand, the Ministry of Health prioritizes Paxlovid for those at highest risk. But if you’re on warfarin or a beta-blocker, Movfor becomes the default. Pharmac (the country’s drug subsidy agency) covers both, so cost isn’t usually a barrier.
Real-World Experience: What Patients Say
One 72-year-old man in Auckland with type 2 diabetes and high blood pressure started Paxlovid after testing positive. He had to stop his cholesterol pill for two weeks. He said the metallic taste was awful, but he didn’t get sick enough to go to the hospital.
A 58-year-old woman on antidepressants couldn’t take Paxlovid. Her doctor gave her Movfor. She had mild nausea but finished the course. She says she felt better faster than her husband, who didn’t take any antiviral.
Another patient, a 45-year-old nurse with asthma, got Remdesivir because she was vomiting and couldn’t keep pills down. She spent three hours in a clinic but didn’t need oxygen. She’s glad she got it.
These stories aren’t rare. They show that the best treatment isn’t always the most effective - it’s the one you can actually take.
When Not to Take Any Antiviral
Antivirals aren’t magic bullets. They don’t help if:
- You’re more than five days into symptoms
- You’re not at high risk for severe disease (young, healthy, fully vaccinated)
- You’re already hospitalized and on oxygen
- You’re pregnant or under 18 (for molnupiravir)
For most healthy people, rest, hydration, and paracetamol are enough. Antivirals are for those who need extra help to avoid the ER.
What’s Next?
New antivirals are in the pipeline. Ensitrelvir is coming to more countries. Long-acting injectables are being tested. But for now, the choices are limited.
If you’re at risk, get tested early. Don’t wait until you’re gasping for air. Call your doctor the moment you test positive. Ask: "Is Paxlovid safe for me? If not, is Movfor an option?" That’s how you make the right call.
Is Movfor better than Paxlovid?
No, Paxlovid is more effective - it reduces hospitalization risk by about 89% compared to Movfor’s 30%. But Movfor is safer for people taking other medications that interact with Paxlovid. The "better" option depends on your health history, not just effectiveness.
Can I take Movfor if I’m pregnant?
No. Movfor (molnupiravir) is not approved for use during pregnancy because animal studies showed potential harm to fetal DNA. Pregnant people with COVID-19 should talk to their doctor about Remdesivir or other safer options.
Does Movfor work against new variants?
Yes. Because molnupiravir targets a part of the virus that doesn’t change much between variants, it remains effective against Omicron sublineages and newer strains. That’s one reason it’s still in use even as vaccines evolve.
How soon after symptoms start should I take Movfor?
Start within five days of symptoms appearing. The earlier, the better - ideally within 48 hours. After five days, the virus has already spread too far for the drug to make much difference.
Can I buy Movfor over the counter?
No. Movfor is a prescription-only medicine in New Zealand and most countries. You need a positive COVID-19 test and a doctor’s assessment of your risk level before it can be dispensed.
Is Movfor still used now that vaccines are widespread?
Yes. Vaccines reduce severe disease, but they don’t eliminate risk - especially for older adults or those with weakened immune systems. Antivirals like Movfor are still part of the standard care for high-risk patients who get infected.
Final Thoughts
Movfor isn’t the best antiviral. But it’s one of the few options when Paxlovid isn’t safe. It’s not perfect - it has limitations, side effects, and safety concerns. But in the right hands, at the right time, it can keep someone out of the hospital. The key is acting fast and knowing your options. Don’t wait. Don’t guess. Talk to your doctor the moment you test positive. Your next steps matter more than you think.

Kathy Pilkinton
October 29, 2025 AT 21:04Let’s be real - Paxlovid is the gold standard, but if you’re on statins or blood thinners, you’re stuck with Movfor like some kind of medical consolation prize. And honestly? The 30% reduction is barely a band-aid when you’ve got a bullet in your chest. Still, better than nothing, I guess. At least they didn’t give me a placebo and call it ‘hope’.
Holly Dorger
October 31, 2025 AT 11:13i read this whole thing and my brain hurt but i think i get it? like movfor is the backup plan when paxlovid says no thanks to your meds. and remdesivir is like the hospital version of a power nap for your immune system. also i dont trust anything that makes the virus copy itself wrong like a drunk student taking notes. lol
Amanda Nicolson
November 1, 2025 AT 21:17Okay so imagine your body is a LEGO castle and the virus is a toddler with a hammer. Paxlovid? That’s the parent who swoops in and takes the hammer away. Movfor? That’s the parent who gives the toddler a broken LEGO piece and says ‘here, build this instead’ - and then the toddler accidentally builds a flamingo that collapses on itself. Remdesivir? That’s the parent dragging the toddler to time-out in a hospital chair for three hours while you cry quietly in the waiting room. It’s not glamorous, but it works. And honestly? I’d take the hospital chair over a broken LEGO flamingo any day.
Jackson Olsen
November 3, 2025 AT 05:02Penny Clark
November 4, 2025 AT 01:32so i had covid last year and my doc gave me movfor bc i was on anxiety med and paxlovid was a no-go. honestly? i felt kinda weird but not worse than the virus. the nausea was annoying but i finished it. my mom took paxlovid and said everything tasted like metal and she cried. i think we all just want to not die. and movfor lets us try.
Niki Tiki
November 5, 2025 AT 21:41Jim Allen
November 7, 2025 AT 13:37Nate Girard
November 8, 2025 AT 14:44Just wanted to say - this post is SO helpful. I’ve been scared to ask my doctor about antivirals because I thought I’d sound dumb. But now I know exactly what to ask: ‘Is Paxlovid safe for me? If not, what’s next?’ That’s the power of clear info. If you’re reading this and you’re high-risk - don’t wait. Call your doctor TODAY. You’ve got options. Use them.
Carolyn Kiger
November 9, 2025 AT 04:35I’m a nurse in rural Nebraska. We don’t have easy access to Paxlovid - sometimes it takes days to get it shipped. Movfor is our go-to. I’ve seen patients who were terrified of the ‘DNA damage’ stuff, but they’d rather take the risk than end up on a ventilator. It’s not perfect, but in places like mine? It’s a lifeline. And honestly? I’m glad it exists.
krishna raut
November 9, 2025 AT 06:52In India, favipiravir is common but not reliable. Stick to what WHO recommends. Movfor and Paxlovid are the only ones worth it. Early treatment matters more than the drug name.