Gout Medications: Allopurinol and Azathioprine Interaction Risks
 Dec, 11 2025
Dec, 11 2025
Allopurinol-Azathioprine Interaction Checker
Check Your Medication Safety
This tool helps you determine if you're taking both medications simultaneously and provides critical safety information about their dangerous interaction.
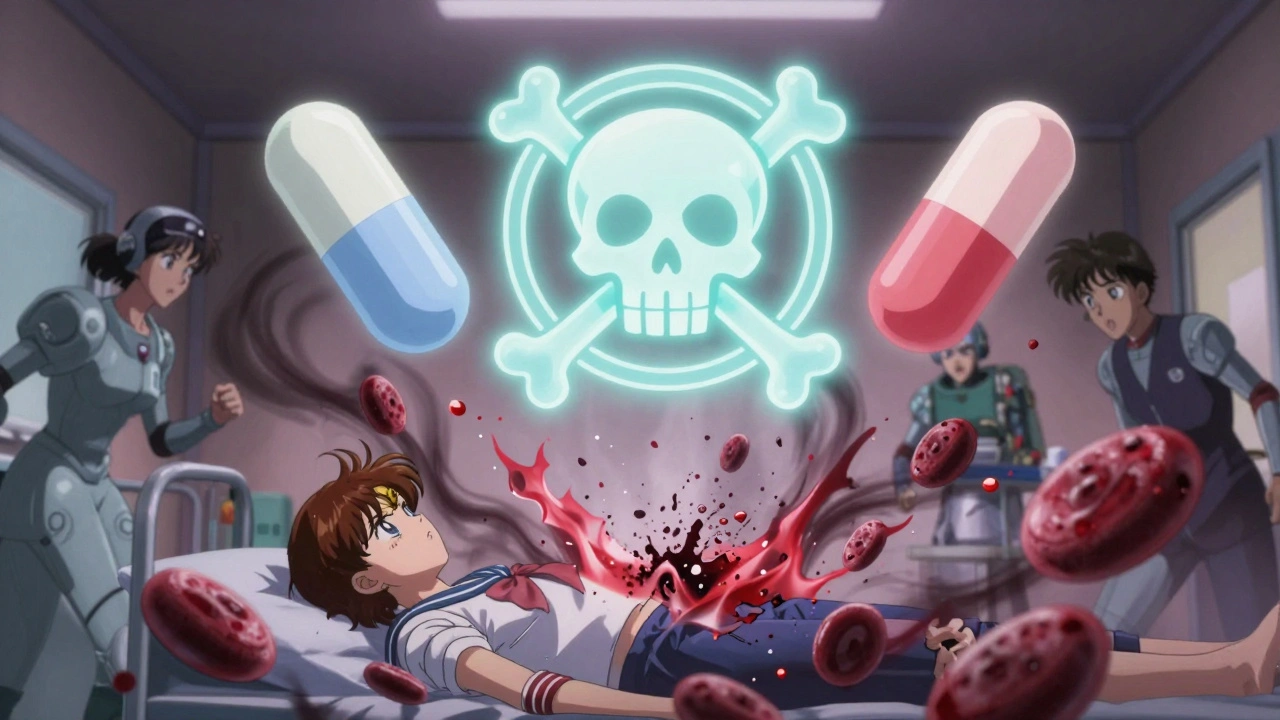
Combining allopurinol and azathioprine can be deadly - and it happens more often than you think. A 63-year-old heart transplant patient in 1996 was prescribed allopurinol for what doctors thought was gout. He was already on azathioprine to prevent organ rejection. Within weeks, his white blood cell count crashed to 1.1 × 10³/mm³. His platelets dropped below 20 × 10³/mm³. He needed blood transfusions and intensive care. The hospital bill? Over $25,000 in today’s money. This isn’t a rare outlier. It’s a textbook example of one of the most dangerous drug interactions in modern medicine.
Why This Interaction Is So Dangerous
Allopurinol is a common gout medication. It lowers uric acid by blocking an enzyme called xanthine oxidase. Azathioprine, on the other hand, is used for autoimmune diseases like Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and after organ transplants. It works by suppressing the immune system. But here’s the problem: azathioprine doesn’t work directly. It turns into 6-mercaptopurine (6-MP) in your body. That’s the real active drug. Xanthine oxidase normally breaks down 6-MP into harmless waste. But when allopurinol blocks that enzyme, 6-MP doesn’t get cleared. Instead, it piles up and gets converted into something far more dangerous - thioguanine nucleotides (6-TGNs). These build up in bone marrow cells, shut down white blood cell production, and trigger cell death. The result? Severe, sometimes fatal, bone marrow suppression. Studies show that when these two drugs are taken together, 6-MP levels can spike by up to four times. That’s not a small increase. That’s enough to turn a safe dose into a lethal one. Patients have been known to develop white blood cell counts so low they can’t fight off a common cold. Platelets drop so far they bleed internally. Hemoglobin levels crash below 4 g/dL - levels that require emergency transfusions.The FDA and Global Health Agencies Say: Avoid This Combo
The U.S. Food and Drug Administration (FDA) put a black box warning on azathioprine packaging - the strongest possible alert. It says clearly: combining azathioprine with allopurinol can cause life-threatening drops in blood cell counts. New Zealand’s Medsafe, the European Medicines Agency, and other global regulators echo this warning. The message is unambiguous: avoid this combination unless you’re under expert supervision. Even so, doctors sometimes miss it. A patient with gout might see their primary care provider. The provider prescribes allopurinol. The patient is also seeing a gastroenterologist for Crohn’s disease and is on azathioprine. Neither doctor knows the other has prescribed something dangerous. The patient takes both. Within weeks, they’re in the hospital. Medsafe’s guidelines say: when you start azathioprine, you must check if the patient is already on allopurinol. That’s not optional. It’s mandatory. Same goes for 6-mercaptopurine - the direct form of the drug. It’s just as dangerous when mixed with allopurinol.There’s One Exception - But Only for Experts
Here’s the twist: there’s a small group of patients who might benefit from this combination - but only under strict control. About 25-30% of people with inflammatory bowel disease (IBD) are called “thiopurine shunters.” Their bodies convert too much azathioprine into a toxic byproduct called 6-MMP, which damages the liver instead of fighting inflammation. They get side effects but no benefit. In these rare cases, adding low-dose allopurinol can redirect the drug’s metabolism. It shuts down the bad pathway (6-MMP) and forces the body to use the good one (6-TGN). A 2018 study of 73 IBD patients showed that when allopurinol was added to a reduced azathioprine dose, 53% went into steroid-free remission. Another 81% were able to stop steroids completely. But here’s the catch: this only works if you reduce azathioprine to 25% of the normal dose - typically from 2-2.5 mg/kg/day down to 0.5-0.75 mg/kg/day. You also need weekly blood tests for the first three months. You need to measure 6-TGN and 6-MMP levels in the blood. You need a specialist who understands thiopurine metabolism. This isn’t something a family doctor can manage. It’s done only in specialized IBD clinics, often with a clinical pharmacist on the team.
What Happens If You Ignore the Warning?
The consequences aren’t theoretical. In 2022, a 57-year-old patient in New Zealand developed pancytopenia after taking both drugs. He had no history of IBD - he was on azathioprine for a kidney transplant. His doctor prescribed allopurinol for gout. No one checked for interactions. He ended up in intensive care. His recovery took months. He lost work. He needed long-term growth factor injections to rebuild his blood cells. Hospital costs for severe myelosuppression from this interaction now exceed $50,000 in the U.S. That’s not just medical bills - it’s lost wages, travel, childcare, time off work. And it’s not always reversible. Some patients never fully recover their bone marrow function.What Should You Do If You’re on One of These Drugs?
If you’re taking azathioprine, 6-mercaptopurine, or cyclophosphamide - and your doctor suggests allopurinol for gout - say no. Ask for alternatives. Febuxostat is another gout medication that doesn’t block xanthine oxidase. It’s safe to use with azathioprine. Pegloticase is another option for severe gout that doesn’t interact at all. If you’re on allopurinol and your doctor starts you on azathioprine - stop. Don’t wait. Call your pharmacist or specialist immediately. Ask: “Is this safe with my current meds?” If you’re a patient with IBD and your doctor mentions combining these two drugs - ask: “Am I a thiopurine shunter? Have you checked my 6-TGN and 6-MMP levels? Are you going to reduce my azathioprine dose? Will you monitor my blood every week?” If they can’t answer confidently, get a second opinion.
Future Changes Are Coming - But Don’t Rely on Them Yet
Researchers are testing genetic tests for TPMT enzyme levels. About 10% of people have low or intermediate TPMT activity, which makes them more vulnerable to this interaction. But these tests aren’t standard everywhere. They’re not fast enough for emergency decisions. And even if you test normal, allopurinol can still push you into danger. New guidelines from the American College of Gastroenterology now conditionally support the combination for shunters - but only in specialized centers. The FDA hasn’t changed its warning. And most primary care doctors still don’t know about it. The bottom line? This interaction is not something to experiment with. It’s not a “maybe.” It’s a hard no - unless you’re in a top-tier IBD clinic with a team that does this every week. Even then, it’s risky.What to Ask Your Doctor
- “Am I taking a drug that interacts with allopurinol?”
- “Is there a safer alternative to allopurinol for my gout?”
- “Have you checked if my current meds include azathioprine or 6-mercaptopurine?”
- “If we must use both, what’s the exact reduced dose? How often will you check my blood?”
- “Can you refer me to a specialist who manages this combination safely?”
Don’t assume your doctor knows. Don’t assume your pharmacist caught it. Don’t assume you’re safe because you’ve been on both for months. This interaction doesn’t wait. It strikes fast. And once it hits, it can change your life forever.

Adam Everitt
December 13, 2025 AT 00:18Audrey Crothers
December 14, 2025 AT 00:02Nathan Fatal
December 14, 2025 AT 03:10Reshma Sinha
December 15, 2025 AT 01:03Ashley Skipp
December 15, 2025 AT 07:03sandeep sanigarapu
December 17, 2025 AT 05:43nikki yamashita
December 18, 2025 AT 10:15Robert Webb
December 20, 2025 AT 03:18Stacy Foster
December 21, 2025 AT 03:31Laura Weemering
December 22, 2025 AT 06:56Levi Cooper
December 22, 2025 AT 15:05