How Medications Treat Heart Rhythm Disorders - A Practical Guide
 Oct, 20 2025
Oct, 20 2025
Heart Rhythm Medication Guide
Select Your Heart Rhythm Condition
This tool helps identify which medication classes are typically used for specific rhythm disorders based on current medical guidelines.
When your heart skips a beat or races unexpectedly, medication can be the first line of defense. Below we break down how different drugs keep the rhythm in check, the science behind each class, and practical tips to use them safely.
What Exactly Is a Heart Rhythm Disorder?
Heart Rhythm Disorders are conditions where the electrical signals that coordinate heartbeats become irregular, too fast, or too slow. Common forms include atrial fibrillation, ventricular tachycardia, and premature beats. In the United States, atrial fibrillation alone affects about 6 million adults and is linked to a 1.5‑fold increase in stroke risk.
Why Medications Matter
While procedures like ablation or device implantation have their place, medications are often the quickest, least invasive way to restore a stable rhythm. They work by either slowing down the electrical impulses, stabilizing cell membranes, or correcting abnormal pathways. For many patients, the right pill can mean fewer hospital visits and a better quality of life.
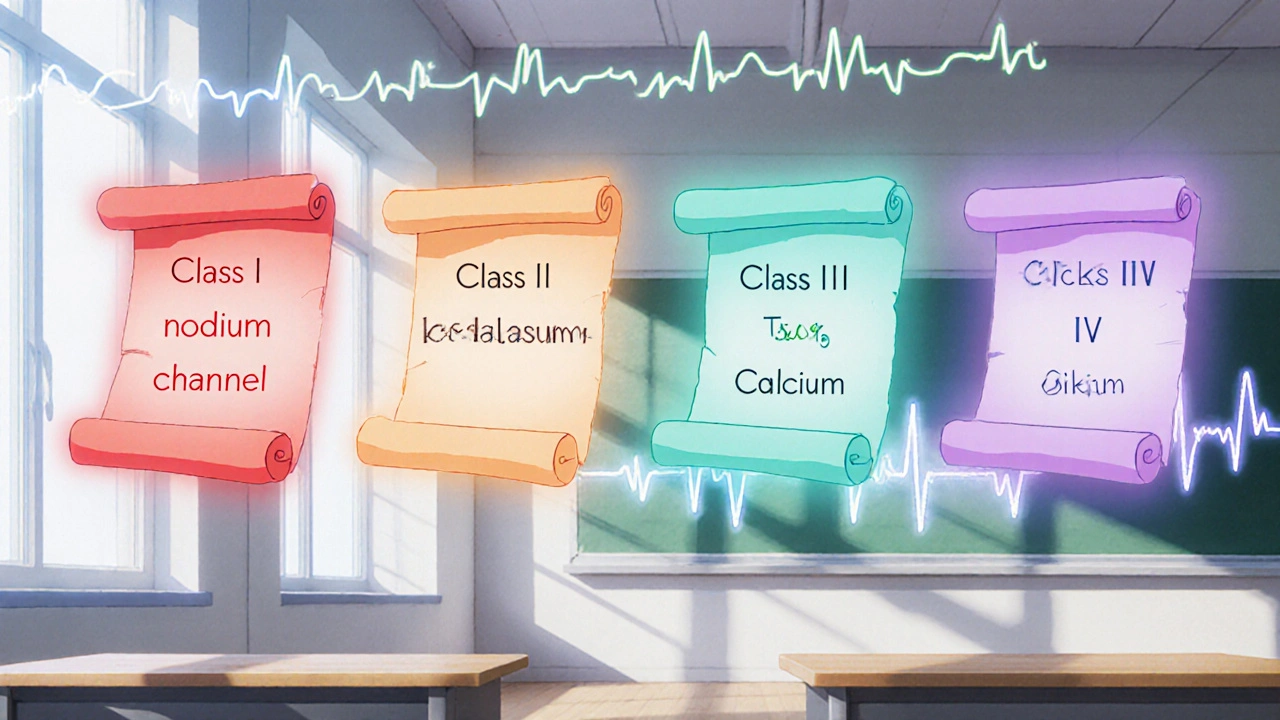
Understanding Antiarrhythmic Medications
Antiarrhythmic Medications are drugs designed specifically to correct abnormal heart rhythms. They fall into four major classes, each targeting a different part of the cardiac electrical system. Knowing which class fits your condition helps doctors choose the safest and most effective option.
| Class | Mechanism | Common Drugs | Typical Use | Main Side Effects |
|---|---|---|---|---|
| Class I - Sodium Channel Blockers | Reduce the rapid influx of sodium during the upstroke of the action potential | Quinidine, Flecainide, Procainamide, Lidocaine, Mexiletine | Often used for ventricular tachycardia (IA, IB) and atrial flutter (IC) | Pro‑arrhythmia, dizziness, GI upset |
| Class II - Beta‑Blockers | Block β‑adrenergic receptors, slowing heart rate and reducing AV‑node conduction | Metoprolol, Atenolol, Carvedilol | Rate control in atrial fibrillation and prevention of recurrent arrhythmias | Fatigue, low blood pressure, bronchospasm |
| Class III - Potassium Channel Blockers | Prolong repolarization by blocking K⁺ channels, extending the refractory period | Amiodarone, Sotalol, Dofetilide, Ibutilide | Broad‑spectrum rhythm control for both atrial and ventricular arrhythmias | Thyroid toxicity (amiodarone), QT prolongation, renal issues |
| Class IV - Calcium Channel Blockers | Inhibit L‑type calcium channels, reducing AV‑node conduction | Diltiazem, Verapamil | Rate control in atrial fibrillation, especially when beta‑blockers are contraindicated | Constipation, bradycardia, heart block |
Matching the Drug to the Disorder
Not every antiarrhythmic works for every rhythm problem. Here’s a quick cheat‑sheet:
- Atrial Fibrillation - Rate control is often first‑line. Beta‑blockers or calcium channel blockers are common, with digoxin added for heart‑failure patients.
- Ventricular Tachycardia - Class I agents like lidocaine or procainamide can stop an acute episode; amiodarone is the go‑to for chronic management.
- Supraventricular Tachycardia (SVT) - Adenosine works for acute termination, while class IC drugs (flecainide) maintain sinus rhythm long‑term.
- Long QT Syndrome - Avoid drugs that prolong QT (many class III agents). Beta‑blockers are protective.
Dosage, Monitoring, and Safety Tips
Even the best drug can backfire without proper monitoring. Here’s what to watch:
- Baseline labs: Kidney and liver function tests guide dosing for drugs like amiodarone and sotalol.
- Electrolytes: Low potassium or magnesium increases the risk of torsades de pointes with class III agents.
- ECG checks: Repeat ECGs after the first dose of any antiarrhythmic to catch QT prolongation early.
- Drug interactions: Many antiarrhythmics are metabolized by CYP450 enzymes. Discuss all over‑the‑counter meds and supplements with your doctor.
- Adherence: Skipping doses can trigger rebound arrhythmias. Set alarms or use a pill organizer.
When Medication Isn’t Enough
Some patients need a backup plan. If you’ve tried multiple drugs without success, doctors may recommend:
- Catheter ablation: Destroys the tissue causing the rogue signals.
- Implantable Cardioverter‑Defibrillator (ICD): Delivers a shock if a life‑threatening rhythm arises.
- Cardiac resynchronization therapy (CRT): Helps the heart pump more efficiently in severe heart‑failure cases.
Common Pitfalls Patients Overlook
Even savvy patients can slip. Watch out for these hidden traps:
- Self‑adjusting doses: Changing your own dose based on how you feel can lead to dangerous swings in heart rate.
- Ignoring lifestyle cues: Caffeine, alcohol, and lack of sleep can blunt medication effectiveness.
- Missing follow‑up appointments: Your doctor needs those lab results to keep the dosage safe.
Key Takeaways
- Heart rhythm disorders range from harmless skips to life‑threatening tachycardias.
- Antiarrhythmic medications are grouped into four classes, each with a specific target in the heart’s electrical system.
- Choosing the right drug depends on the type of arrhythmia, existing health conditions, and potential side‑effects.
- Regular labs, ECG monitoring, and strict adherence are critical for safety.
- If drugs fail, procedural options like ablation or ICDs become the next step.
Frequently Asked Questions
Can antiarrhythmic drugs cure atrial fibrillation?
They can restore normal rhythm in many patients, but "cure" is a strong word. Atrial fibrillation often recurs, so long‑term medication or periodic monitoring is usually needed.
What’s the biggest safety concern with amiodarone?
Amiodarone can affect the thyroid, lungs, liver, and eyes. Regular blood tests and chest X‑rays are essential, especially after the first six months.
Are beta‑blockers safe for people with asthma?
Selective beta‑1 blockers (like metoprolol) are generally safer than non‑selective ones, but anyone with asthma should discuss options with their doctor.
How quickly do antiarrhythmic drugs work?
Some, like IV lidocaine, act within minutes for acute episodes. Oral drugs such as sotalol may take several days to reach steady‑state levels.
Do lifestyle changes reduce the need for medication?
Yes. Maintaining a healthy weight, limiting alcohol, and managing stress can lower the frequency of arrhythmia episodes, often allowing lower drug doses.
Understanding how heart rhythm disorder medications work empowers you to partner with your healthcare team, ask the right questions, and stay ahead of potential complications. With the right drug, the right dose, and diligent follow‑up, most people can keep their hearts beating in a steady, healthy rhythm.

Sakib Shaikh
October 20, 2025 AT 23:55Listen up, folks-these antiarrhythmic drugs ain't just magic pills, they're the frontline knights battling the chaos inside your heart. Class I agents slam the sodium gates like a rock‑concert door, while Class III prolongs the repolarization so the rogue signals lose their rhythm. You think a little dizziness is nothing? It’s your body screaming that the electrophysiology is being reshaped, and you better respect the dosage. Missed a dose? Expect a rebound that feels like the heart's doing a freestyle rap on a broken beat. And don’t even get me started on amiodarone’s long‑term side‑effects-thyroid, lungs, eyes, the whole circus. So keep those labs tight and your cardiologist on speed‑dial, or you’ll be swimming in more than just blood.
Ashok Kumar
October 26, 2025 AT 17:48Oh sure, because everyone loves a good heart‑shaking surprise at 3 am. At least the doctors warned you about the possible dizziness.
Jasmina Redzepovic
November 1, 2025 AT 12:41From a cardiological standpoint, the electrophysiological modulation achieved by Class III potassium channel blockers exemplifies the pinnacle of pharmacologic engineering-an achievement predominantly refined within American research institutions. The pharmacokinetic profile of amiodarone, characterized by a massive volume of distribution and hepatic cytochrome P450‑mediated metabolism, necessitates vigilant therapeutic drug monitoring to avert iatrogenic toxicity. Moreover, the pro‑arrhythmic potential inherent to Class I sodium channel antagonists underscores the necessity for genotype‑guided therapy, a paradigm our nation is uniquely poised to implement on a large scale.
Esther Olabisi
November 7, 2025 AT 07:35Wow, look at that fancy talk-so fancy you need a PhD just to read the label 😂. Good thing we’ve got the basic stuff like “take it with food” to keep things simple.
Dana Yonce
November 13, 2025 AT 02:28💡 A quick tip: checking your potassium levels before starting a Class III drug can save you from a scary QT stretch 🚀. Keep that electrolyte balance tight and the heart will thank you.
erica fenty
November 18, 2025 AT 21:21Indeed; baseline labs are essential; monitor QTc regularly; adjust dosage per pharmacodynamics!!!
Xavier Lusky
November 24, 2025 AT 16:15What they don’t tell you is that the FDA’s approval process for antiarrhythmics is riddled with hidden agendas, and the data you see in journals is often skewed to favor big pharma’s profits.
Ivan Laney
November 30, 2025 AT 11:08When you dive deep into the realm of cardiac electrophysiology, you quickly realize that antiarrhythmic therapy is not a one‑size‑fits‑all solution, but rather a meticulously calibrated orchestra of ion channel modulation and autonomic balance. Class I sodium channel blockers, such as flecainide and procainamide, act by attenuating the rapid upstroke of phase 0, thereby slowing conduction velocity in both atrial and ventricular tissue. However, their pro‑arrhythmic risk, especially in patients with structural heart disease, demands careful patient selection and often a concurrent beta‑blocker regimen to blunt sympathetic triggers. Moving on to Class II agents, beta‑blockers like metoprolol and carvedilol provide rate control by dampening catecholamine‑mediated AV‑node conduction, a mechanism that is particularly valuable in atrial fibrillation with rapid ventricular response. The elegance of Class III potassium channel inhibitors lies in their ability to prolong the action potential duration, expanding the refractory period and thus preventing re‑entry circuits; yet this same prolongation can precipitate torsades de pointes if electrolytes are not meticulously maintained. Amiodarone, the heavyweight champion of the class, boasts a broad spectrum of efficacy but carries a notorious adverse‑effect profile, ranging from thyroid dysfunction to pulmonary fibrosis, necessitating lifelong surveillance with thyroid panels and chest imaging. Calcium channel blockers of Class IV, such as diltiazem and verapamil, selectively target L‑type channels, offering a middle ground for rate control when beta‑blockers are contraindicated, but they must be used cautiously in patients with compromised left ventricular function. The practical aspect of therapy extends beyond the pharmacodynamics: dosing intervals, formulation choices between oral and IV routes, and potential drug–drug interactions via CYP3A4 metabolism all shape the clinical outcome. Electrolyte management, especially potassium and magnesium repletion, cannot be overstated, as even marginal deficiencies amplify the risk of QT prolongation and subsequent ventricular tachyarrhythmias. Moreover, genetic polymorphisms in ion channel genes are emerging as critical determinants of drug response, heralding an era of personalized antiarrhythmic therapy that may eventually render the trial‑and‑error approach obsolete. Patient adherence remains the cornerstone of success; missed doses can trigger rebound arrhythmias that are often more refractory than the initial episode. Lifestyle modifications-from limiting caffeine and alcohol intake to ensuring adequate sleep-complement pharmacologic strategies and often reduce the required drug burden. Finally, the decision matrix should always incorporate the possibility of non‑pharmacologic interventions, such as catheter ablation or implantable cardioverter‑defibrillators, when medication alone fails to achieve durable rhythm control.
Kimberly Lloyd
December 6, 2025 AT 06:01In the grand tapestry of health, each medication is a thread that, when woven with intention and mindfulness, creates a rhythm of life that sings louder than any arrhythmia could ever disrupt.
Chirag Muthoo
December 12, 2025 AT 00:55It is advisable to schedule quarterly follow‑up appointments to reassess therapeutic efficacy and safety.
Angela Koulouris
December 17, 2025 AT 19:48Think of those check‑ups as vibrant pit stops-fueling your heart’s journey with fresh insights and keeping the engine humming beautifully.