Hypocalcemia and Osteoporosis: Key Facts You Need to Know
 Oct, 4 2025
Oct, 4 2025
Hypocalcemia & Osteoporosis Risk Calculator
Risk Assessment Results
Key Risk Factors Identified:
Recommendations:
Symptom Comparison
- Tingling around mouth or fingertips
- Muscle cramps or spasms
- Seizures (in severe cases)
- Cardiac irregularities
- Height loss over 2 cm after age 50
- Back pain from compression fractures
- Fragility fractures from minor falls
- Loss of posture or stooped appearance
Low blood calcium and weak bones might seem like separate health issues, but they’re closely linked. Understanding how hypocalcemia can set the stage for osteoporosis helps you catch problems early and take the right steps to protect your skeleton.
Key Takeaways
- Hypocalcemia reduces the calcium available for bone formation, often triggering hormonal changes that speed up bone loss.
- Vitamin D, parathyroid hormone (PTH) and dietary calcium are the three main players in the calcium‑bone loop.
- Blood tests, bone mineral density (BMD) scans and symptom checks are essential to spot both conditions.
- Correcting calcium levels, ensuring adequate vitamin D, and adopting bone‑friendly habits can halt or reverse the progression toward osteoporosis.
- Medication such as bisphosphonates is useful when lifestyle changes aren’t enough, but they work best after calcium and vitamin D are optimized.
What Is Hypocalcemia?
Hypocalcemia is a medical condition where the concentration of calcium in the blood falls below the normal range (typically under 8.5 mg/dL). Calcium is vital for nerve signaling, muscle contraction, and blood clotting, so when levels dip, the body can react with tingling sensations, muscle cramps, or even cardiac irregularities.
What Is Osteoporosis?
Osteoporosis is a chronic bone disease marked by reduced bone mass and structural deterioration, making bones fragile and more prone to fractures. The condition often goes unnoticed until a minor fall results in a broken hip or wrist.
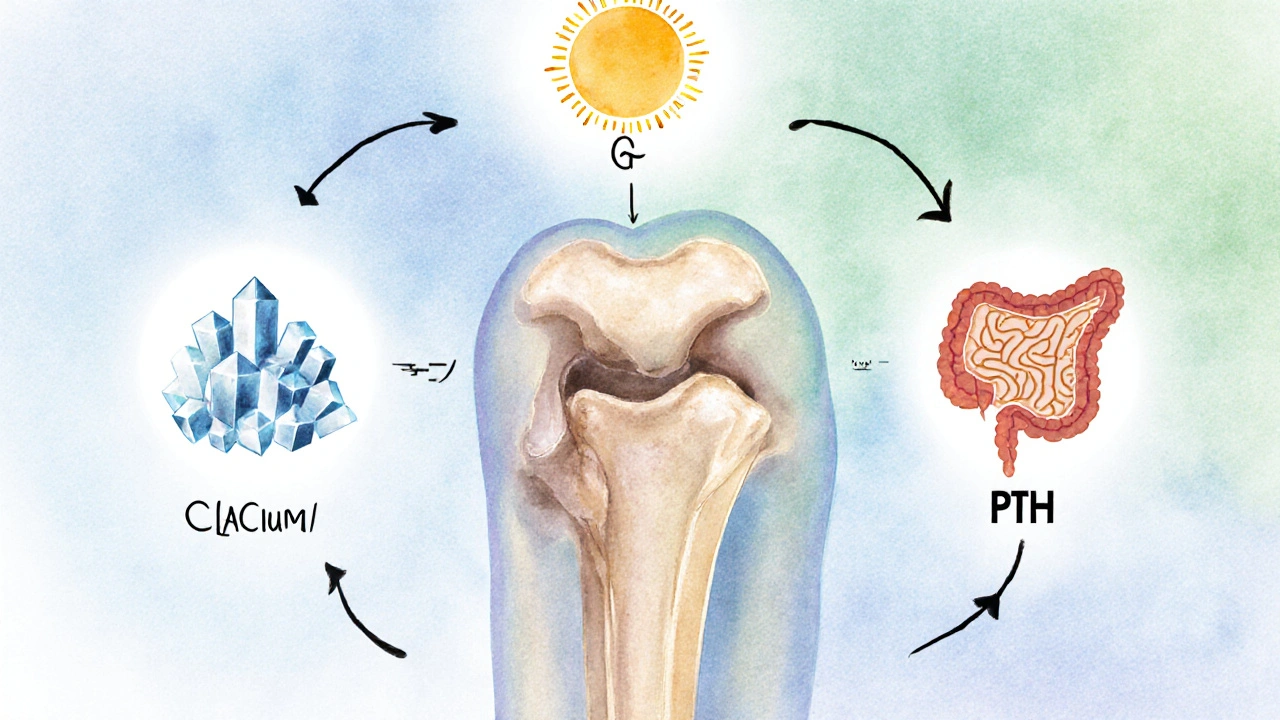
Calcium, Vitamin D, and Parathyroid Hormone: The Bone Trio
Three core components keep the calcium‑bone system balanced:
- Calcium supplies the mineral matrix that gives bone its strength.
- Vitamin D boosts intestinal absorption of calcium and supports bone mineralization.
- Parathyroid hormone (PTH) acts as the emergency regulator: when blood calcium drops, PTH spikes, prompting bones to release calcium into the bloodstream.

The Physiological Link: From Low Calcium to Bone Loss
When hypocalcemia develops, the parathyroid glands release more PTH to restore normal calcium levels. This surge of PTH:
- Stimulates osteoclasts - the cells that break down bone tissue - to release calcium stored in bone.
- Reduces renal calcium excretion, conserving what’s left in the blood.
- Encourages the kidneys to convert vitamin D into its active form, calcitriol, to improve calcium absorption.
While these mechanisms are life‑saving in the short term, chronic elevation of PTH causes continuous bone resorption. Over months and years, the net loss of bone density can culminate in osteoporosis.
Shared Risk Factors
Several lifestyle and medical factors push both hypocalcemia and osteoporosis in the same direction:
- Inadequate dietary calcium - common in low‑dairy or vegan diets without fortified foods.
- Vitamin D deficiency - caused by limited sun exposure, darker skin tones, or malabsorption disorders.
- Age‑related decline in gut absorption and renal activation of vitamin D.
- Medications such as glucocorticoids, proton‑pump inhibitors, and certain anticonvulsants.
- Chronic kidney disease, which impairs conversion of vitamin D and excretion of phosphate, worsening calcium imbalance.
Symptoms and Diagnosis
Because hypocalcemia and osteoporosis have overlapping and subtle symptoms, a combined diagnostic approach is essential.
Hypocalcemia clues include:
- Tingling around the mouth or fingertips (paresthesia).
- Muscle cramps or tetany.
- Seizures in severe cases.
Osteoporosis clues are often silent, but common signs are:
- Height loss greater than 2cm after age 50.
- Back pain from vertebral compression fractures.
- Fragility fractures from low‑impact falls.
Laboratory tests for calcium, ionized calcium, PTH, and 25‑hydroxy vitamin D give a biochemical snapshot. For bone health, doctors rely on Bone mineral density (BMD) measured by dual‑energy X‑ray absorptiometry (DEXA) scans. A T‑score of −2.5 or lower confirms osteoporosis.
Management Strategies
Treating the two conditions together yields the best outcomes.
1. Replenish Calcium
- Aim for 1,000mg/day for adults under 50, and 1,200mg/day for those over 50 (higher for men with high bone turnover).
- Choose calcium carbonate (requires stomach acid) or calcium citrate (better for older adults on acid‑suppressing meds).
2. Optimize Vitamin D
- Target serum 25‑hydroxy vitamin D of 30-50ng/mL.
- Supplement 800-1,000IU/day for most adults; up to 2,000IU/day for those with proven deficiency.
3. Address Secondary Hyperparathyroidism
If PTH stays high after calcium and vitamin D correction, clinicians may use calcimimetics or consider surgical evaluation of the parathyroid glands.
4. Lifestyle Moves
- Weight‑bearing exercises - brisk walking, dancing, resistance training - boost osteoblast activity.
- Avoid excessive caffeine and sodium, which increase urinary calcium loss.
- Quit smoking and limit alcohol to two drinks per day.
5. Pharmacologic Options for Osteoporosis
When lifestyle changes aren’t enough, Bisphosphonates such as alendronate or risedronate inhibit osteoclasts, slowing bone loss and reducing fracture risk.
Comparison of Symptoms: Hypocalcemia vs. Osteoporosis
| Feature | Hypocalcemia | Osteoporosis |
|---|---|---|
| Primary system affected | Neuromuscular (tingling, cramps) | Skeletal (fragile bones) |
| Typical onset | Acute or sub‑acute after diet/med changes | Gradual, often silent for years |
| Diagnostic test | Serum calcium, ionized calcium, PTH | DEXA BMD scan, T‑score |
| Common triggers | Low dietary calcium, vitamin D deficiency, certain drugs | Age, hormonal changes, long‑term steroid use |
| Management focus | Calcium/VitD repletion, treat PTH excess | Bone‑strengthening meds, exercise, nutrition |

Frequently Asked Questions
Can correcting low calcium prevent osteoporosis?
Yes, restoring normal calcium levels reduces the stimulus for excess PTH release, which in turn lessens bone‑resorbing activity. However, other factors like vitamin D, hormonal status and lifestyle still play crucial roles.
What blood test values indicate hypocalcemia?
A total serum calcium below 8.5mg/dL (2.12mmol/L) or ionized calcium under 4.6mg/dL signals hypocalcemia. Labs often also report elevated PTH if the body is trying to compensate.
Is a DEXA scan needed for everyone with low calcium?
Not every patient, but a DEXA scan is recommended when low calcium coexists with other risk factors (age >50, family history, prior fractures) to assess bone density early.
Can supplements alone cure osteoporosis?
Supplements are a foundation, but osteoporosis usually requires a combined approach: adequate calcium and vitaminD, regular weight‑bearing exercise, and, in many cases, prescription medicines like bisphosphonates.
What foods are best for raising calcium levels?
Dairy products (milk, yogurt, cheese), fortified plant milks, leafy greens (kale, bokchoy), sardines with bones, and calcium‑set tofu are top choices. Pair them with vitaminD‑rich foods like fatty fish or egg yolks for better absorption.

Anthony MEMENTO
October 4, 2025 AT 17:00Listen up the calcium industry doesn’t want you to connect the dots between low blood calcium and bone loss.
They hide the fact that many supplements are laced with cheap fillers.
Every time you read about osteoporosis you see a glossy ad for a calcium pill.
The truth is the body’s own regulation via parathyroid hormone is being hijacked by hidden toxin exposure.
Chronic low calcium triggers PTH to gnaw away at bone to restore serum levels.
That mechanism is exactly why you end up with fragile skeletons.
What they don’t tell you is that the same hormone surge can cause kidney stones and heart rhythm issues.
The data from independent labs shows a correlation between low vitamin D regions and higher fracture rates.
Yet the pharma lobby pushes vitamin D as a “nice‑to‑have” rather than essential.
If you look at historical bone density charts you see a steady decline after the 1970s when processed foods exploded.
Processed foods are low in bioavailable calcium and high in phosphates that further suppress absorption.
The hidden agenda is to create a market for both calcium and bisphosphonate drugs.
You can break the cycle by eating real dairy, leafy greens and exposing skin to sunlight.
Stop believing the convenient narrative and demand real blood work before any prescription.
Your bones will thank you when you restore the natural balance.
aishwarya venu
October 4, 2025 AT 19:13I totally get how overwhelming it can feel navigating calcium and bone health.
It’s encouraging to see that simple diet tweaks and sunlight can make a huge difference.
Keep sharing these practical tips everyone will benefit.
Nicole Koshen
October 4, 2025 AT 21:26Calcium homeostasis is a tightly regulated system and any disruption can ripple through bone metabolism.
When serum calcium drops, parathyroid hormone spikes, leading to increased osteoclast activity which over time reduces bone mineral density.
It’s crucial to monitor both serum levels and vitamin D status to catch the imbalance early.
Ed Norton
October 4, 2025 AT 23:40Good point Nicole, concise and clear.
Karen Misakyan
October 5, 2025 AT 01:53In the realm of osteo‑metabolic disorders, a comprehensive appraisal of calcium–vitamin D–parathyroid interplay is indispensable.
The literature unequivocally demonstrates that secondary hyperparathyroidism precipitates net bone resorption, thereby accelerating osteoporotic progression.
Accordingly, therapeutic regimens must prioritize repletion of calcium stores and optimization of 25‑hydroxyvitamin D concentrations prior to pharmacologic intervention.
Moreover, employing dual‑energy X‑ray absorptiometry affords a quantifiable metric of skeletal integrity, facilitating risk stratification.
It is incumbent upon clinicians to adopt a multimodal strategy that amalgamates nutritional, lifestyle, and pharmacologic modalities.
Amy Robbins
October 5, 2025 AT 04:06Sure Karen, because everyone has time to schedule a DEXA before their morning coffee.
Also, note that “repletion” is not a word you’d find in a kitchen recipe.
Let’s keep the grammar pristine while we’re at it.
Shriniwas Kumar
October 5, 2025 AT 06:20The calcium–phosphate axis operates within a sophisticated endocrinological framework where homeostatic feedback loops modulate osteoclastic resorption via PTH‑mediated signaling cascades.
Dysregulation at the molecular tier, often precipitated by suboptimal nutraceutical intake, culminates in phenotypic osteopenic manifestations.
Jennifer Haupt
October 5, 2025 AT 08:33Your exposition elegantly elucidates the mechanistic cascade, yet it also invites contemplation on the broader epistemic implications of nutritional autonomy versus medical determinism.
By empowering patients with evidence‑based knowledge, we transcend mere symptom management and foster holistic wellbeing.
NANDKUMAR Kamble
October 5, 2025 AT 10:46What if the very guidelines we follow are engineered by hidden lobbies to keep us dependent on endless supplements?
The pattern of recurring recommendations feels orchestrated.
namrata srivastava
October 5, 2025 AT 13:00Indeed, the perpetuation of such prescriptive norms reflects an entrenched paradigm of biomedical hegemony, wherein subtle coercion masquerades as benign counsel.
Priyanka arya
October 5, 2025 AT 15:13This breakdown of calcium dynamics is absolutely mind‑blowing 🤯.
Loren Kleinman
October 5, 2025 AT 17:26When one considers the intricate symphony of calcium flux, vitamin D activation, and parathyroid hormone modulation, it becomes apparent that the skeletal system is not merely a static scaffold but rather a dynamic organ whose structural integrity is perpetually negotiated through a delicate balance of mineral deposition and resorptive processes, a balance that, if perturbed by chronic hypocalcemia, initiates a cascade of osteoclastic activity that over years erodes trabecular and cortical bone, ultimately manifesting clinically as osteoporosis, a condition that underscores the necessity of proactive nutritional strategies, regular biomechanical loading exercises, and periodic densitometric assessments to preemptively identify and mitigate bone loss.
Sabrina Goethals
October 5, 2025 AT 19:40Wow, Loren, that's a thorough explanation, and it really highlights how many factors intertwine, from diet to hormones, to lifestyle, and even genetics, making bone health such a complex, yet fascinating, topic.
Sudha Srinivasan
October 5, 2025 AT 21:53People ignore calcium deficiencies at their own peril.
Jenny Spurllock
October 6, 2025 AT 00:06Exploring the calcium‑vitamin D‑PTH loop reveals how each component supports the others, creating a self‑regulating system essential for skeletal health.
Bart Cheever
October 6, 2025 AT 02:20Another article about calcium, same old stuff.