Parkinson’s DBS: How Deep Brain Stimulation Works and Who Benefits Most
 Dec, 4 2025
Dec, 4 2025
What Deep Brain Stimulation Actually Does for Parkinson’s
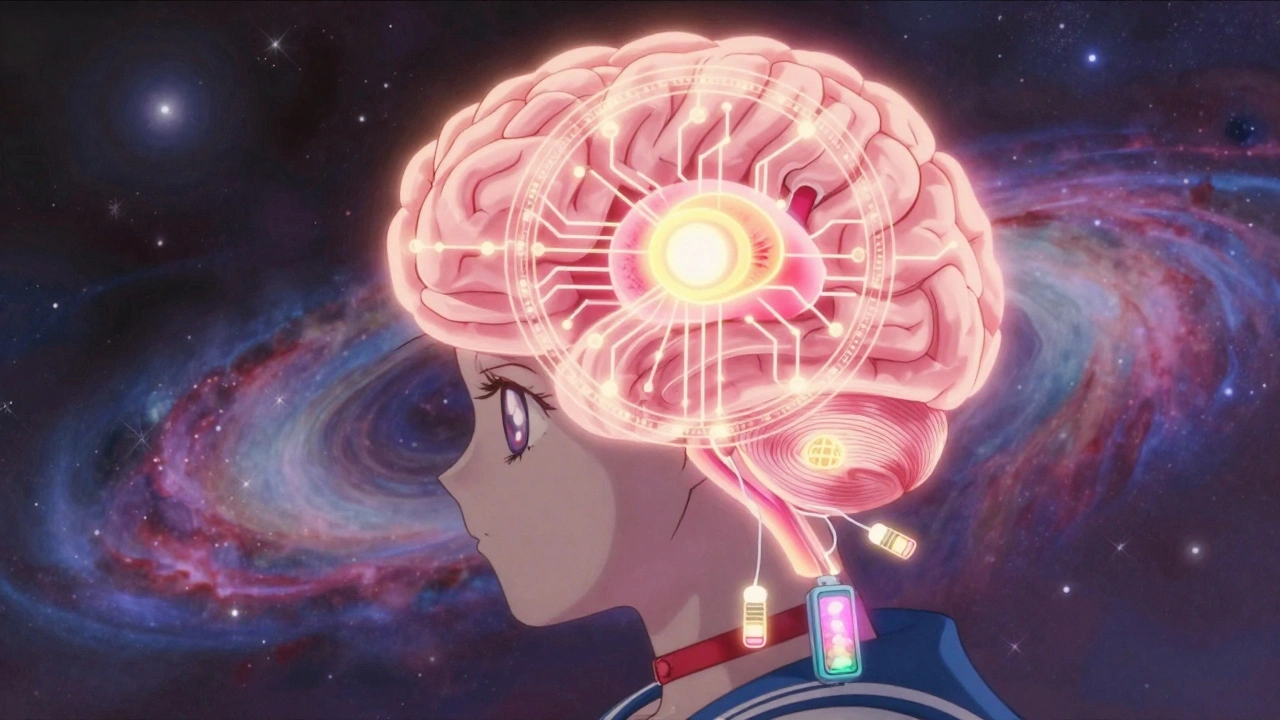
Deep Brain Stimulation, or DBS, isn’t a cure for Parkinson’s. It doesn’t stop the disease from progressing. But for many people, it changes everything. If your tremors won’t stay still, your meds cause wild swings between freezing up and shaking uncontrollably, or you’re tired of swallowing pills every hour - DBS can help. It works by sending tiny electrical pulses to specific parts of the brain that control movement. These pulses don’t kill brain cells. They don’t remove anything. They just reset the noisy signals that cause Parkinson’s motor symptoms.
Think of it like a pacemaker for your brain. Surgeons implant thin wires (electrodes) into areas like the subthalamic nucleus or globus pallidus. These connect to a small battery pack, usually placed under the skin near your collarbone or abdomen. The device runs 24/7, adjusting the brain’s abnormal electrical activity. The result? Up to 80% reduction in dyskinesias, 60-80% less time spent in "off" states, and often a 30-50% drop in daily levodopa doses. The EARLYSTIM trial showed patients who got DBS early in their disease course improved their quality of life scores by 23 points - more than double what medication alone could do.
Who Is a Good Candidate for DBS?
Not everyone with Parkinson’s is a candidate. The biggest red flag? If your symptoms don’t improve when you take levodopa, DBS won’t help much. That’s because DBS only works on symptoms that respond to medication. If you’re stiff and slow when you’re off meds, but feel almost normal after a dose - you’re likely a good fit. Studies show people with this kind of response see 60-70% improvement after surgery. Those with atypical parkinsonism - like progressive supranuclear palsy or multiple system atrophy - usually get less than 10% benefit.
There are hard rules. Most centers require at least 5 years of Parkinson’s symptoms. You need to show a 30% or better improvement on the UPDRS-III motor scale after taking levodopa. Your cognitive score must be above 24 on the MMSE or 21 on the MoCA. If you’re struggling with memory, planning, or decision-making, DBS can make it worse. Depression and anxiety are okay if they’re managed, but untreated psychiatric issues are a dealbreaker.
Age isn’t a hard cutoff, but most patients are between 55 and 75. Older patients can still benefit, but recovery takes longer and risks like infection or bleeding rise slightly. The real deciding factor? How much Parkinson’s is limiting your life. If you can’t walk without freezing, can’t button your shirt, or avoid social events because you’re embarrassed by shaking - DBS might be worth considering.
STN vs GPi: Which Brain Target Is Right for You?
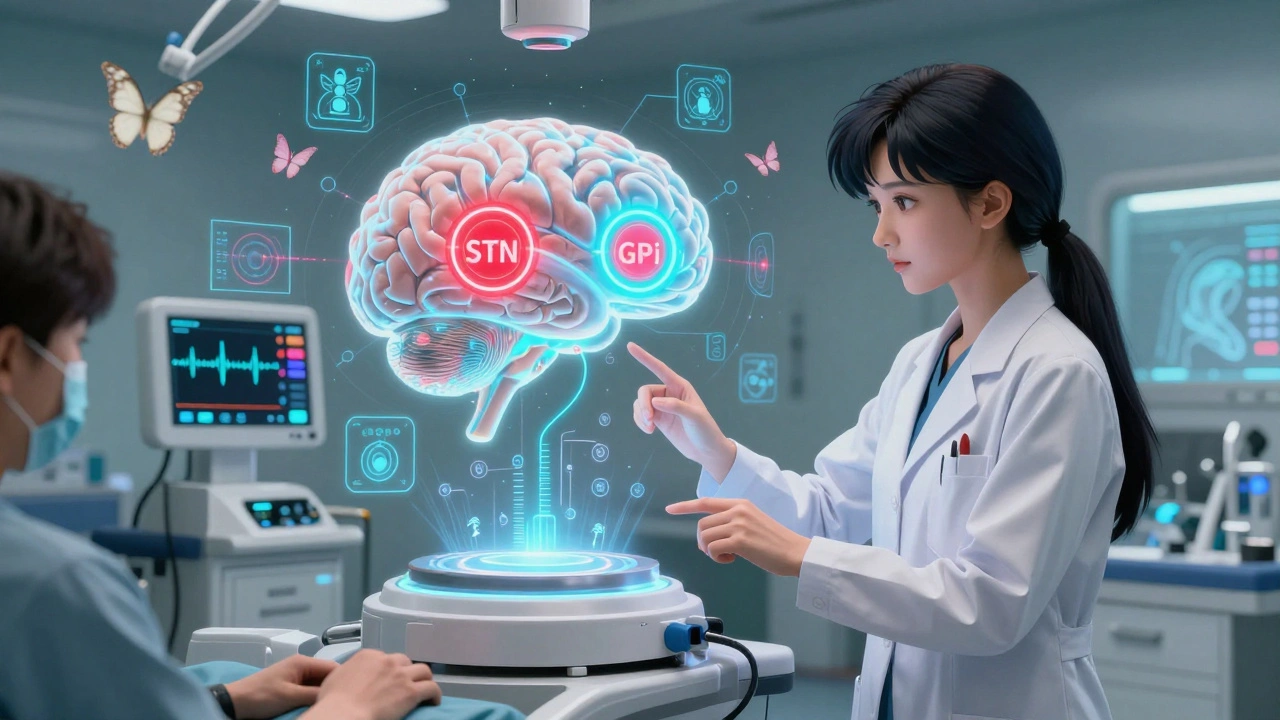
There are two main spots surgeons target: the subthalamic nucleus (STN) and the globus pallidus interna (GPi). Both work well for tremors and stiffness. But they have different trade-offs.
STN lets you cut your medication dose more - often by half. That means fewer side effects like nausea, hallucinations, or sudden drowsiness. But it comes with a risk: some people report more trouble with speech, word-finding, or mood. One Reddit user wrote: "My tremors vanished, but now I forget words mid-sentence. It’s frustrating." GPi doesn’t reduce meds as much, but it’s better at controlling dyskinesias - the involuntary movements caused by long-term levodopa use. It also has fewer cognitive side effects. If you’re already struggling with memory or focus, GPi might be the safer pick. The VA/NINDS trial found GPi reduced dyskinesias by 70% compared to 46% with STN.
There’s no one-size-fits-all answer. Your neurologist and surgeon will look at your symptoms, your meds, your personality, and your goals. If you want to cut pills and stay active, STN makes sense. If your biggest problem is uncontrollable jerking, GPi might be better. Many centers now use advanced imaging and real-time brain recordings to pick the best target for your brain.
The Real Cost - Money, Time, and Recovery
DBS isn’t cheap. In the U.S., the total cost runs between $50,000 and $100,000. That includes surgery, hospital stay, the device, and the first year of programming. Medicare and most private insurers cover it if you meet criteria, but getting approval can take 3-6 months. You’ll need proof you’ve tried and failed on multiple medication regimens.
Then there’s time. The whole process takes 3-6 months. First, you see a movement disorder specialist. Then neuropsych testing - 4-6 hours of memory, attention, and mood tests. You’ll get a high-res 3T MRI. Then a team meeting: neurologist, neurosurgeon, psychologist, and sometimes a speech therapist. If approved, surgery takes 3-6 hours. You’re awake during part of it so the team can test your responses. Recovery takes 4-6 weeks. You won’t turn the device on right away - it usually starts 2-4 weeks post-op.
Programming is where the real work begins. It’s not like flipping a switch. It takes 6-12 months of fine-tuning. You’ll need monthly visits at first. You’ll track your symptoms in a diary: when you’re stiff, when you shake, when meds kick in. Your clinician adjusts voltage, frequency, and pulse width. Some newer devices, like Medtronic’s Percept™ PC, even record brain signals and auto-adjust. But most still need human input. And if your battery isn’t rechargeable, you’ll need another surgery every 3-5 years to replace it.
What No One Tells You About Life After DBS
Most people feel like they’ve gotten their life back. But the reality is messier.
Positive stories are common: "I can hug my grandkids without shaking." "I went back to gardening." "I stopped hiding in the house." One patient from the EARLYSTIM trial said, "I didn’t realize how much I’d lost until I got it back." But there are surprises. Some people lose their ability to multitask. Planning a meal, organizing a trip, even remembering a grocery list can take longer. Speech can become quieter or slurred. Balance and walking - especially freezing episodes - often don’t improve much. DBS doesn’t fix everything. And it doesn’t stop non-motor symptoms like constipation, sleep issues, or depression.
Some patients feel disappointed because they expected a cure. One forum post read: "I thought DBS would stop the disease. It didn’t. It just made my good days better." Hardware problems happen too. About 5-15% of people need a revision surgery - for infection, broken wires, or lead movement. Battery failures, though rare, can cause sudden loss of benefit. That’s why regular check-ups are non-negotiable.
Why So Few People Get DBS - Even When They Should
Here’s the shocking part: only 1-5% of people who qualify for DBS actually get it. Why?
Many doctors don’t bring it up. They assume patients won’t want surgery. Or they wait too long - until the disease is too advanced. The Parkinson’s Foundation calls DBS "markedly underutilized." Patients often don’t know it exists. Some think it’s experimental. Others fear brain surgery.
But the data is clear. If you’ve had Parkinson’s for 5+ years, your meds aren’t working well, and you’re still responsive to levodopa - you’re likely a candidate. And the earlier you get it, the better. The EARLYSTIM trial showed patients who got DBS earlier (after 4 years) had better long-term outcomes than those who waited until symptoms were severe.
Center volume matters too. Hospitals that do more than 50 DBS procedures a year have 20% fewer complications. Look for a movement disorder center with a dedicated DBS team - neurologist, neurosurgeon, neuropsychologist, and a coordinator who helps you through the whole process.
What’s Next for DBS?
The field is moving fast. The newest devices can "listen" to your brain. Medtronic’s Percept™ PC records beta waves - the brain signals linked to Parkinson’s stiffness - and adjusts stimulation automatically. Early results show 27% better symptom control than old-school DBS.
Researchers are testing DBS for non-motor symptoms: depression, anxiety, even memory issues. One 2023 study found people with the LRRK2 gene mutation respond 15% better to DBS. That could mean future selection isn’t just about symptoms - it could be about your DNA.
And there’s talk of using DBS earlier - even after just 3 years of symptoms. The EARLYSTIM-2 trial is exploring this now. If it works, we might stop thinking of DBS as a last resort. It could become a standard tool, like insulin for diabetes.
Final Thoughts: Is DBS Right for You?
DBS isn’t magic. But for the right person, it’s life-changing. It doesn’t fix everything. It doesn’t stop the disease. But it can give you back hours of your day, reduce your pill burden, and let you do things you thought were gone for good.
If you’re considering it, start with your neurologist. Ask: "Do I still respond to levodopa?" "Have I had Parkinson’s for at least 5 years?" "Am I still cognitively sharp?" If the answers are yes, ask for a referral to a DBS center. Don’t wait until you’re too far gone. The best outcomes come from early, thoughtful selection - not desperation.
It’s a big decision. But for thousands of people, it was the best one they ever made.
Can DBS cure Parkinson’s disease?
No, DBS does not cure Parkinson’s. It doesn’t stop the brain cells from dying or slow disease progression. It only treats the motor symptoms - like tremors, stiffness, and dyskinesias - that respond to levodopa. People still need to take medication, though often at lower doses. Non-motor symptoms like sleep problems, constipation, and mood changes usually don’t improve.
How long does the DBS battery last?
Battery life depends on the device. Non-rechargeable batteries last 3-5 years and require replacement surgery. Rechargeable systems, like Medtronic’s Percept™ PC or Boston Scientific’s Vercise™ Genus™, last 9-15 years. You’ll need to charge them regularly - usually a few hours once or twice a week. Rechargeable devices are now standard for most new patients.
Will I still need to take Parkinson’s meds after DBS?
Yes, but usually much less. Most patients reduce their levodopa dose by 30-50%. STN targets allow bigger reductions than GPi. Some people can cut their pills in half. But you can’t stop completely - DBS doesn’t replace medication. It works alongside it. Missing doses can still cause symptoms to return.
What are the biggest risks of DBS surgery?
The main risks are bleeding in the brain (1-3% chance), infection (2-5%), and hardware problems like broken wires or lead movement (5-15%). There’s also a small risk of stroke, seizure, or speech problems. Most complications are treatable. Serious permanent damage is rare. Choosing a high-volume center (>50 procedures/year) cuts your risk by 20%.
How long does it take to see results from DBS?
You won’t feel changes right after surgery. The device is usually turned on 2-4 weeks later. Improvements in tremor and stiffness often show up within days. But fine-tuning takes months. Most people reach their best settings after 6-12 months of programming visits. Patience is key - it’s not instant, but the gains are lasting.
Can DBS help with balance and walking problems?
Not reliably. DBS helps tremors, stiffness, and dyskinesias - but axial symptoms like freezing, balance loss, and shuffling gait respond poorly. Only 20-30% improvement is typical. This is one of DBS’s biggest limitations. Research is ongoing, but current devices aren’t designed to fix these issues well. Physical therapy and fall prevention remain critical.
Is DBS safe for older patients?
Age alone isn’t a barrier. Many patients over 70 benefit. But recovery takes longer, and risks like infection or bleeding rise slightly. The key is overall health - not age. If you’re otherwise fit, mentally sharp, and have strong support at home, DBS can be safe and effective. Centers now routinely evaluate patients in their 70s and even early 80s.
What happens if the DBS device stops working?
If the device fails - battery dies, wire breaks, or infection occurs - symptoms will return to their pre-DBS state. That’s why regular check-ups matter. Most modern systems have alerts for low battery or malfunction. If you notice sudden worsening of symptoms, contact your team immediately. Most hardware issues can be fixed with a minor procedure. Don’t wait until you’re completely off.

Lynette Myles
December 5, 2025 AT 02:24Annie Grajewski
December 6, 2025 AT 00:38Harry Nguyen
December 6, 2025 AT 19:15Philip Kristy Wijaya
December 6, 2025 AT 22:46Jennifer Patrician
December 7, 2025 AT 21:24Mellissa Landrum
December 8, 2025 AT 02:27luke newton
December 9, 2025 AT 14:11Ali Bradshaw
December 9, 2025 AT 22:20an mo
December 11, 2025 AT 14:13aditya dixit
December 11, 2025 AT 21:01William Chin
December 11, 2025 AT 23:54Ada Maklagina
December 12, 2025 AT 06:30Stephanie Fiero
December 13, 2025 AT 04:22sean whitfield
December 14, 2025 AT 01:30