Respiratory Combination Inhalers: What You Need to Know About Generic Substitution
 Feb, 12 2026
Feb, 12 2026
When you’re managing asthma or COPD, your inhaler isn’t just a device-it’s your lifeline. But what happens when your pharmacy swaps your branded inhaler for a generic version without warning? For many patients, this switch isn’t just a cost-saving move-it’s a hidden risk. Unlike pills, where a generic drug works the same way no matter the brand, respiratory combination inhalers depend heavily on the device itself. And that’s where things get dangerous.
Why Your Inhaler Isn’t Just a Drug
Respiratory combination inhalers deliver two medicines in one puff: usually a corticosteroid to reduce inflammation and a long-acting beta agonist to open your airways. Brands like Symbicort Turbohaler and Advair Diskus have been the gold standard for years. But now, generics are flooding the market. The first generic versions hit shelves around 2019-2020 after patents expired. Sounds good, right? Cheaper meds mean more people can afford treatment. But here’s the catch: these generics aren’t just different pills. They come in different devices. The Turbuhaler uses a twisting motion to load a dose. The Spiromax uses a side slider. The Diskus requires a sharp inhale. The Flexhaler needs a firm click before you breathe in. If you’ve been using one for years, switching to another without training can mean your medication never reaches your lungs. A 2020 study found that 76% of patients switched from a Turbuhaler to a Spiromax without proper instruction used the device incorrectly. That’s not a small number. That’s four out of five people. And when your inhaler doesn’t work right, your asthma gets worse-not better.The Device Difference: How Delivery Changes Everything
There are three main types of inhalers: pressurized metered-dose inhalers (pMDIs), dry powder inhalers (DPIs), and nebulizers. Each works differently. pMDIs need perfect timing-you press the canister and breathe in slowly at the same time. DPIs? You need to inhale fast and hard to pull the powder out. If you don’t, the medicine sticks in your mouth or throat. No effect. Just money wasted. The problem isn’t the medicine. It’s the delivery. Studies show that even when the active ingredients are identical, lung deposition can vary by 25-40% between devices. That’s like taking a 10-mg dose and only getting 6 mg into your lungs. That’s not a little less. That’s not enough. A 2021 study in the Journal of Aerosol Medicine and Pulmonary Drug Delivery found that patients switched from Symbicort Turbohaler to a generic Spiromax without training had a 22% spike in asthma attacks within six months. That’s not a coincidence. That’s a direct result of improper technique.Global Rules, Different Outcomes
Regulations vary wildly. In the U.S., the FDA says if a generic inhaler is approved, it’s interchangeable. You don’t need training. You don’t need to be told. Just swap it. But in Europe, the European Medicines Agency (EMA) requires proof that the generic delivers the same amount of medicine to the lungs as the original. That means clinical studies, not just chemical tests. The UK’s NICE guidelines are even clearer: “Switching inhaler devices without a consultation may be associated with worsened asthma control.” They’ve seen it happen too often. In Germany, pharmacists must give 15 minutes of in-person training to every new inhaler user. In the U.S., only 28% of pharmacies offer any device training at all. And it shows. Norway has a 62% generic substitution rate for inhalers. France? Only 22%. Why? Because France requires doctors to prescribe by brand name. No substitution allowed. It’s not about cost. It’s about safety.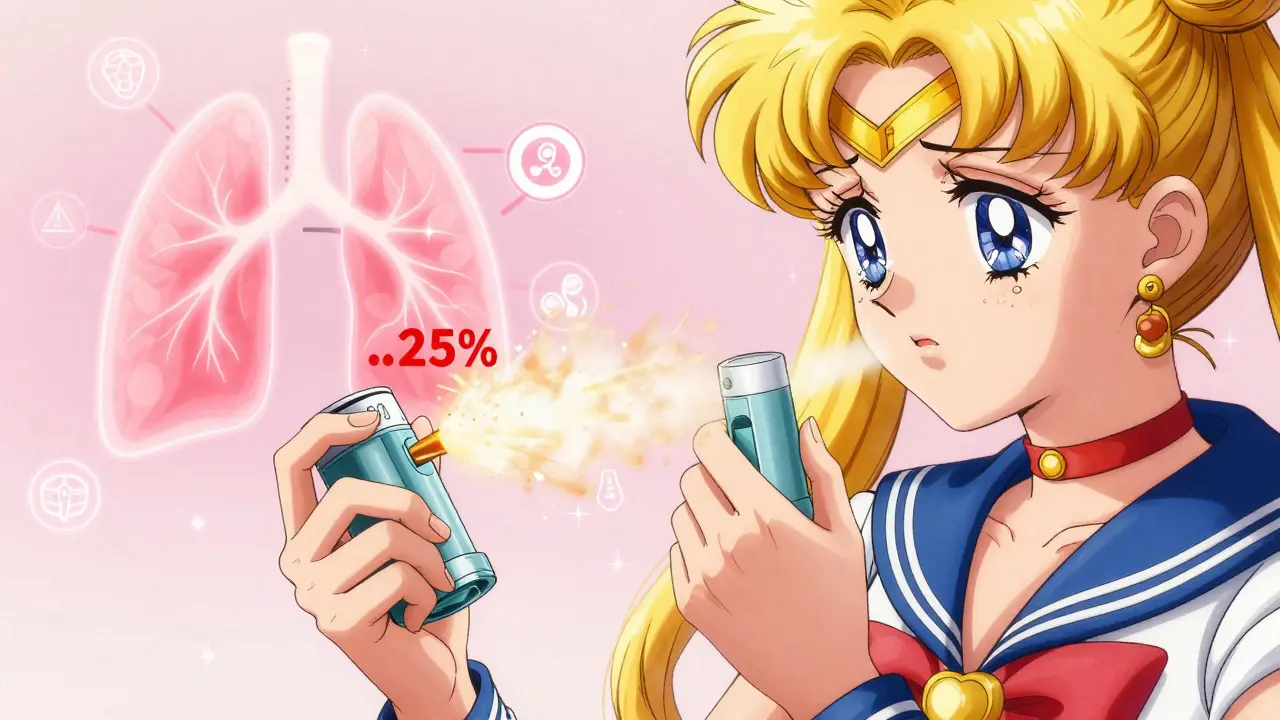
What Patients Are Saying
On Reddit’s r/asthma community, 83% of 82 people who were switched to a generic inhaler without warning reported worse symptoms. One user wrote: “I didn’t know I had to breathe harder. I thought the inhaler was broken. My asthma got so bad I ended up in the ER.” A 2022 survey by Asthma UK of 1,247 people found that 57% felt confused after switching devices. Of those, 32% went to the emergency room within three months. On Drugs.com, Symbicort Turbohaler has a 6.2/10 rating. The generic Spiromax? 4.8/10. The top complaints? “Harder to use,” “Feels less effective,” “Different technique required.” But here’s the good news: when patients get proper training, 89% use the new device correctly. It’s not the generic that’s the problem. It’s the lack of instruction.What Should You Do?
If your pharmacy switches your inhaler:- Ask if it’s the same device. If not, ask why.
- Request a demonstration. Don’t just watch-do it yourself. Use the teach-back method: show your pharmacist or nurse how you use it. If you mess up, they correct you right away.
- Ask for written instructions. A picture or diagram helps more than words.
- Check the label. If the device looks different, don’t assume it works the same.
- Track your symptoms. If you feel worse in the first few weeks, call your doctor. Don’t wait.


Sophia Nelson
February 12, 2026 AT 20:21