Silent Gallstones: Detection and Treatment Guide
 Oct, 18 2025
Oct, 18 2025
Silent Gallstone Risk Assessment Tool
This tool estimates your risk of developing symptoms from asymptomatic gallstones based on key clinical factors. Results are for educational purposes only and shouldn't replace medical advice.
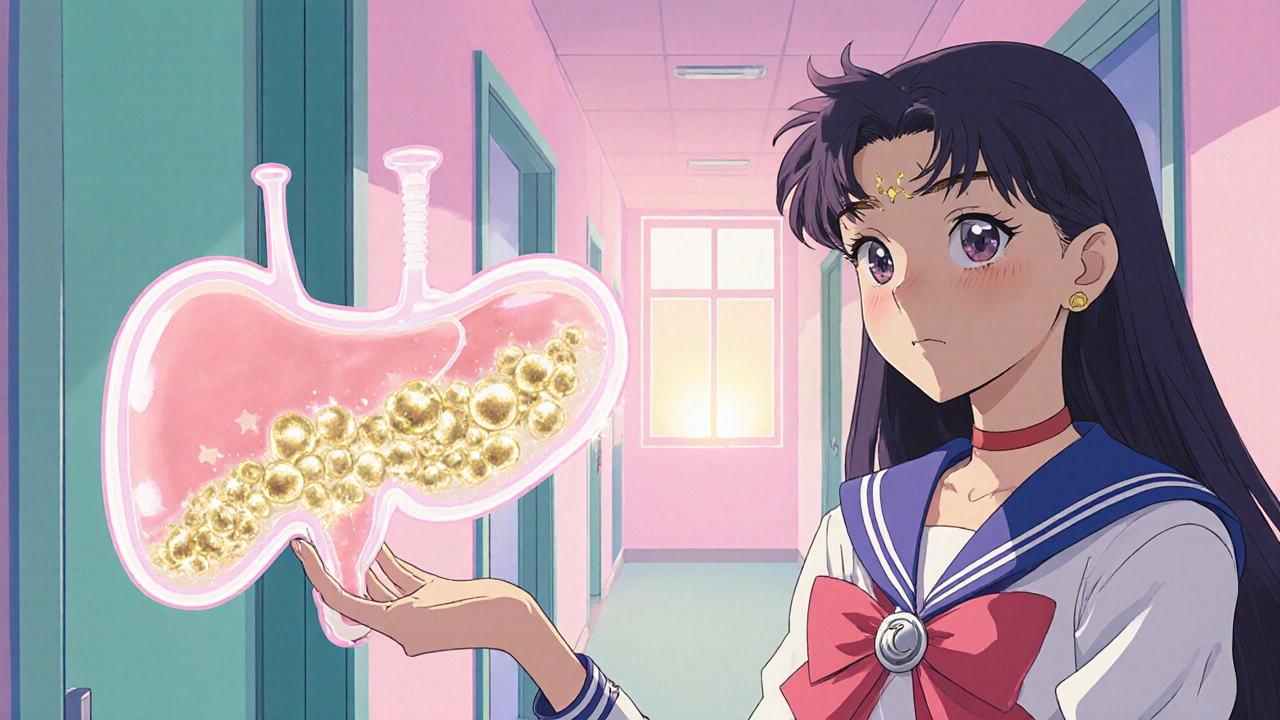
When it comes to Gallstones-solid, pebble‑like deposits that form in the gallbladder-, most people picture sudden pain after a greasy meal. But a surprising number of stones never announce themselves. They sit quietly, sometimes for years, and only reveal their presence during a routine scan or when a complication finally forces a symptom.
Key Takeaways
- Silent gallstones are asymptomatic stones that often hide until discovered by imaging.
- Risk climbs with obesity, rapid weight loss, certain diets, and genetics.
- Ultrasound is the first‑line detection tool; CT and MRCP are useful for complex cases.
- Treatment ranges from watchful waiting to minimally invasive surgery, based on stone size and patient health.
- Lifestyle tweaks-balanced diet, steady weight, and regular activity-can lower future stone formation.
What Exactly Are Silent Gallstones?
Most gallstones cause a classic colicky pain known as Biliary colic-a sudden, intense ache in the upper right abdomen. Silent gallstones, however, never trigger this flare‑up. They remain asymptomatic, meaning patients feel nothing at all. The stones are still there, often measuring less than 5 mm, and can still block the bile duct if they move.
Because there’s no pain, the condition is frequently missed until an unrelated abdominal ultrasound spots the stones, or until a serious complication like Choledocholithiasis-the presence of stones in the common bile duct causes jaundice or infection.
Who Is Most at Risk?
Anyone can develop gallstones, but research shows that several factors increase the odds of a silent case:
- Obesity: Excess body fat raises cholesterol in bile, encouraging stone formation.
- Rapid weight loss: Diets that drop more than 1 kg per week can make the liver secrete extra cholesterol.
- Female gender and pregnancy: Hormonal changes slow gallbladder emptying.
- Age: Risk climbs after 40, and silent stones become more common in seniors.
- Dietary risk factors: High‑fat, low‑fiber diets and frequent intake of refined carbs add fuel to the fire.
Family history also plays a role; if a close relative had gallstones, you’re more likely to develop them, silent or not.
Why Do They Hide?
Silent stones are usually small and stay lodged in the gallbladder rather than the bile duct. The gallbladder can accommodate a few pebble‑sized stones without enough pressure to trigger pain receptors. Additionally, some people have a high pain threshold or an atypical nerve pathway, so even a blocked duct may not produce noticeable discomfort.
In many cases, the only clue is a subtle change in lab results-slightly elevated liver enzymes-or a vague feeling of fullness after meals. Because these signs are easily brushed off, the condition can linger unnoticed for years.
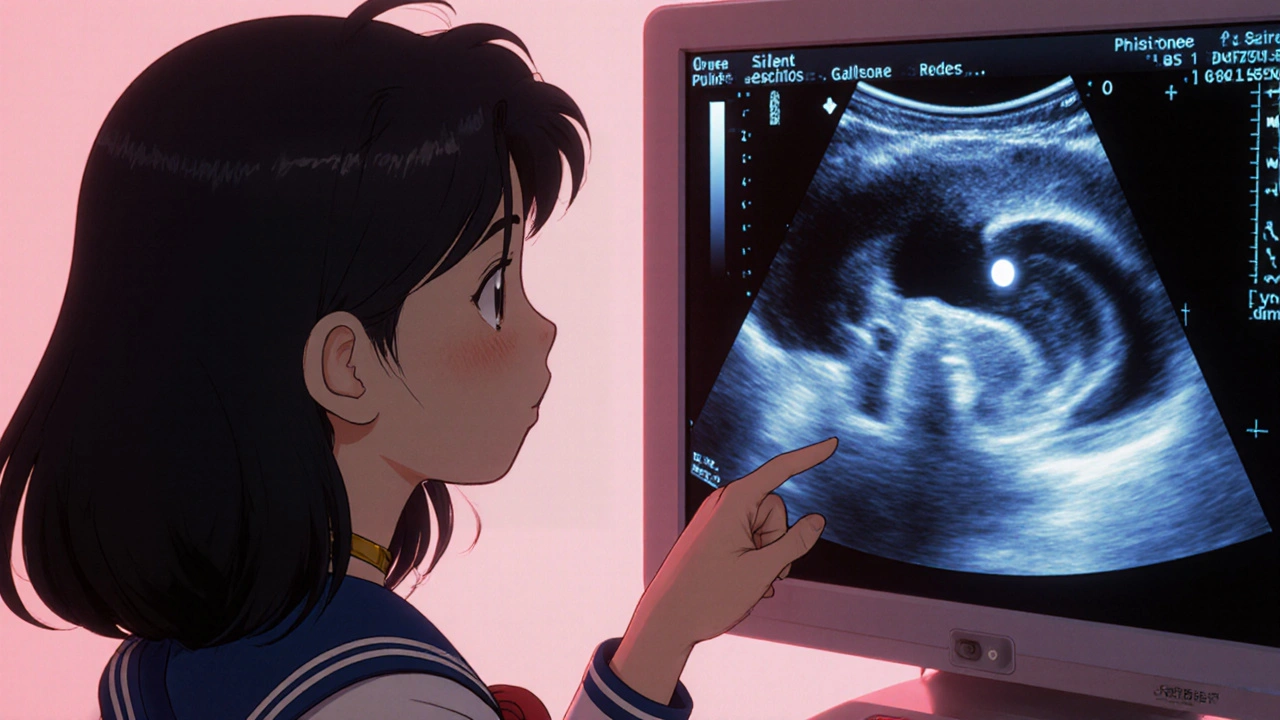
How to Detect Silent Gallstones
Detection hinges on a combination of clinical suspicion, blood work, and imaging. Here’s the usual workflow:
- Physical exam: Doctors may feel a tender area beneath the right rib cage, but often the exam is normal.
- Blood tests: Elevated bilirubin, alkaline phosphatase, or liver transaminases can hint at a bile flow problem.
- Imaging: This is where silent stones reveal themselves.
The imaging arsenal includes several tools, each with strengths and drawbacks. Below is a quick comparison:
| Method | Best For | Pros | Cons |
|---|---|---|---|
| Ultrasound‑uses high‑frequency sound waves to image the gallbladder | Initial screening, small stones | Non‑invasive, no radiation, cheap | Operator‑dependent, may miss tiny stones |
| CT scan‑provides cross‑sectional images with radiation | Complicated anatomy, large stones | High detail, good for emergency settings | Radiation exposure, less sensitive to tiny stones |
| MRCP‑magnetic resonance cholangiopancreatography, visualizes bile ducts | Assessing ductal stones, surgical planning | No radiation, excellent duct detail | Costly, longer exam time |
| ERCP‑endoscopic procedure that can image and remove stones | Therapeutic removal of ductal stones | Both diagnostic and therapeutic | Invasive, risk of pancreatitis |
For most silent cases, a simple abdominal Ultrasound catches the stones. If the ultrasound is inconclusive or if a doctor suspects a stone has slipped into the common bile duct, they may order a CT scan or MRCP for clearer images.
Treatment Options: From Watching to Operating
The big question once stones are found is: "Do I need to do something?" The answer depends on stone size, location, patient age, and overall health.
- Watchful waiting: If stones are tiny (<5 mm) and the patient has no symptoms, many doctors recommend a "wait and see" approach, with yearly ultrasounds.
- Medication: Oral bile‑acid pills like ursodeoxycholic acid can gradually dissolve cholesterol stones, but the process takes months and works best for small, cholesterol‑rich stones.
- Non‑surgical procedures: ERCP can extract stones lodged in the bile duct without open surgery.
- Best for ductal stones causing jaundice.
- Risk of pancreatitis, so it’s not first‑line for silent gallbladder stones.
- Surgical removal: The definitive cure is Laparoscopic cholecystectomy, a keyhole surgery that removes the gallbladder.
- Less than 2‑hour procedure, short hospital stay.
- Recovery in 1‑2 weeks for most people.
- Recommended for stones larger than 5 mm, repeated episodes, or high‑risk patients.
Most silent stone patients eventually opt for surgery after a few years, especially if they develop any discomfort or if the stones grow.
Lifestyle Tweaks to Keep Stones at Bay
Even after removal, the underlying risk factors can cause new stones. Here are practical steps that actually move the needle:
- Balanced diet: Aim for 45‑55% carbs, 20‑25% healthy fats, and 20‑25% protein. Load up on fiber (fruits, veg, whole grains) to help bile flow.
- Steady weight loss: If you need to lose weight, keep it to 0.5‑1 kg per week. Crash diets spike cholesterol in bile.
- Hydration: Drinking at least 2 L of water daily helps keep bile thin.
- Limit refined sugars and trans fats: These raise triglycerides and promote stone formation.
- Regular movement: Even a brisk 30‑minute walk daily improves gallbladder motility.
When to Seek Medical Help
Silent stones are called "silent" for a reason, but they can turn loud fast. Call a doctor if you notice:
- Sudden, severe pain in the upper right abdomen or back.
- Yellowing of skin or eyes (jaundice).
- Fever, chills, or a rapid heartbeat-possible infection.
- Dark urine or clay‑colored stools.
These signs suggest a stone has moved into the bile duct or caused a blockage, and prompt treatment can prevent serious complications like pancreatitis.
Quick Checklist for Patients
- Know your risk factors (obesity, rapid weight loss, family history).
- Get an abdominal ultrasound if you have any vague abdominal discomfort.
- Review blood work for subtle liver enzyme changes.
- Discuss treatment thresholds with your doctor-size, symptoms, overall health matter.
- Adopt a gallstone‑friendly lifestyle to reduce recurrence.
Can silent gallstones cause complications?
Yes. Even without pain, stones can migrate into the common bile duct, leading to jaundice, infection, or pancreatitis. That’s why routine imaging for high‑risk people is essential.
How accurate is ultrasound for detecting silent gallstones?
Ultrasound picks up about 95% of stones larger than 3 mm. Small cholesterol stones under 2 mm may be missed, so a follow‑up CT or MRCP is advised if suspicion remains.
Is medication effective for silent gallstones?
Oral bile‑acid therapy can dissolve cholesterol stones under 5 mm, but success rates hover around 30‑50% and treatment can take 6‑24 months. It’s best for patients who cannot undergo surgery.
When is surgery the preferred option?
Surgery is advised when stones are larger than 5 mm, cause repeated episodes, or sit in the bile duct. Laparoscopic cholecystectomy offers a cure with minimal downtime.
Can lifestyle changes prevent new stones after surgery?
Absolutely. Maintaining a healthy weight, eating high‑fiber meals, and avoiding rapid crash diets keep bile composition balanced, reducing the chance of new stone formation in the remaining biliary system.

Nhasala Joshi
October 18, 2025 AT 21:29The silent gallstone conspiracy is far more insidious than any mainstream health article will admit 😱.
The governments and big pharma collude to keep the public oblivious, branding these stones as “asymptomatic” to avoid costly surgeries.
They hide behind polite medical jargon like ultrasound and MRCP while the real agenda is to push people toward expensive laparoscopic procedures.
Every time a routine scan uncovers a stone, it's a little victory for the hidden elite who profit from the follow‑up interventions.
The epidemiological data cited in reputable journals are deliberately cherry‑picked, masking the fact that silent stones can linger for decades without causing pain.
Patients with high cholesterol, rapid weight loss, or even a genetic predisposition are told to ‘watchful waiting’ – a euphemism for the healthcare system’s inertia.
But the truth is that these stones act as ticking time‑bombs, ready to erupt into choledocholithiasis the moment you least expect it.
If you glance at the liver enzyme panels, the subtle rise in alkaline phosphatase is a covert SOS signal that most physicians ignore.
The ultrasound machines, touted as low‑cost and non‑invasive, are calibrated to miss sub‑5‑mm stones unless the operator is specifically instructed to look for them.
That is why some private imaging centers boast higher detection rates – they have been instructed to expose the hidden threat.
Meanwhile, the pharmaceutical lobby pushes cholesterol‑lowering meds that merely mask the symptom‑free stone formation.
Dietary advice about balanced meals and steady weight loss is a distraction, a glossy PR campaign to shift responsibility back onto the patient.
If you truly want to protect yourself, demand a high‑resolution MRCP even if the ultrasound is negative.
Insist on a second opinion and keep a personal log of any vague fullness after meals, because the silent stones rarely announce themselves.
Only through relentless vigilance can we outsmart the conspiratorial silence that surrounds gallstone detection 🕵️♂️.
Stay aware, question the guidelines, and share this knowledge before the next stone slips unnoticed.
Emma Williams
October 18, 2025 AT 22:40Great info, thanks for sharing.
Alex Lineses
October 19, 2025 AT 00:03Ultrasound remains the frontline tool for detecting silent gallstones, and its accessibility makes it ideal for routine checks.
If you have risk factors like obesity or rapid weight loss, schedule an annual abdominal scan.
Early detection can prevent complications such as choledocholithiasis, which often requires more invasive procedures.
Keep an eye on your liver function tests; subtle elevations may hint at biliary obstruction.
Remember, proactive monitoring is the best strategy to stay ahead of potential issues.
kendra mukhia
October 19, 2025 AT 01:26Only a fool would ignore the glaring red flags presented by modern imaging standards, and yet many patients remain blissfully unaware.
The medical establishment’s half‑hearted ‘watchful waiting’ approach is nothing more than a lazy band‑aid for a deeper systemic failure.
If you truly care about your health, you must demand a high‑resolution MRCP and refuse to settle for vague reassurance.
Bethany Torkelson
October 19, 2025 AT 02:50Stop making excuses and get the scan done now!
Your body is literally harboring foreign objects and you act as if it’s normal.
Wake up, take control, and schedule that MRCP before the stones decide to strike.
Grace Hada
October 19, 2025 AT 04:13Silent gallstones epitomize the hidden paradox of the body: unseen yet potent.
Recognition demands both intellect and vigilance.
alex montana
October 19, 2025 AT 05:36Wow!! this!!! is!!! insane????? you see?? the?? ultrasound?? sometimes? misses? stones??
Wyatt Schwindt
October 19, 2025 AT 07:00I appreciate the thorough breakdown; it's helpful for anyone navigating this condition.
Lyle Mills
October 19, 2025 AT 08:23From a hepatobiliary perspective, integrating serial transabdominal ultrasonography with periodic MRCP offers a stratified diagnostic algorithm that optimizes sensitivity while minimizing radiation exposure.
Barbara Grzegorzewska
October 19, 2025 AT 09:46This article is a veritable masterpiece of med‑knowledge, delving into the clandestine realm of silent cholelithiasis with a flourish that would make even the most seasoned gastroenterologists swoon.
The blend of clinical insight and lifestyle guidance feels almost too perfect, as if the authors had a secret agenda to educate us all.
Sarah Hanson
October 19, 2025 AT 11:10Thank you for the comprehensive overview; the emphasis on lifestyle modification is particularly valuable.
Brian Van Horne
October 19, 2025 AT 12:33Honestly, I’m just glad to finally learn why my occasional post‑meal fullness wasn’t ‘nothing’ – now I’ll keep an eye on my diet and get checked when it feels right.