Clinical Outcomes Data: What Studies Tell Providers About Generics
 Feb, 1 2026
Feb, 1 2026
When a patient walks into your office with a prescription for a brand-name drug, you might wonder: is the generic version really just as good? It’s a question that comes up often - not because providers doubt the science, but because real-world experience can feel messy. Patients report feeling different. Pharmacists swap pills without warning. Insurance companies push generics hard. And then there’s the fear: what if switching hurts someone?
Generics aren’t cheap knockoffs - they’re rigorously tested
The truth is, every generic drug approved in the U.S. has gone through a process more controlled than most people realize. The FDA doesn’t just compare labels. It requires proof that the generic delivers the same active ingredient, in the same amount, at the same rate, as the brand-name version. That’s called bioequivalence. For most drugs, that means the amount of medicine in the bloodstream (measured as AUC and Cmax) must fall within 80-125% of the brand’s levels. For drugs with narrow therapeutic windows - like warfarin, levothyroxine, or tacrolimus - the standard is even tighter, using scaled methods that account for individual patient variability.And it works. A 2019 study in PLOS Medicine looked at over 1.3 million patient pairs across 14 different conditions. For 12 of those, there was no meaningful difference in clinical outcomes between generic and brand-name drugs. In fact, for amlodipine and amlodipine/benazepril, patients on generics had slightly better cardiovascular outcomes. That’s not a fluke. It’s data - and it’s consistent across cardiovascular, metabolic, and neurological drugs.
Where things get complicated - and why it matters
Not all drugs behave the same. Psychiatric medications show a small but noticeable pattern: some studies report slightly higher rates of psychiatric hospitalization with generics. For escitalopram and sertraline, hazard ratios hovered around 1.05-1.07. At first glance, that sounds alarming. But dig deeper. The same study found that even when patients switched from brand-name to authorized generics (made by the original brand company), hospitalization rates didn’t drop. That suggests it’s not the drug - it’s perception.Patients expect to feel different when a pill changes color, shape, or size. Even if the active ingredient is identical, the psychological shift can trigger real symptoms. One study showed patients on generics were no more likely to stop taking their meds than those on brand-name drugs. But when they did stop, they often blamed the generic - even when the real issue was cost, side effects, or poor counseling.
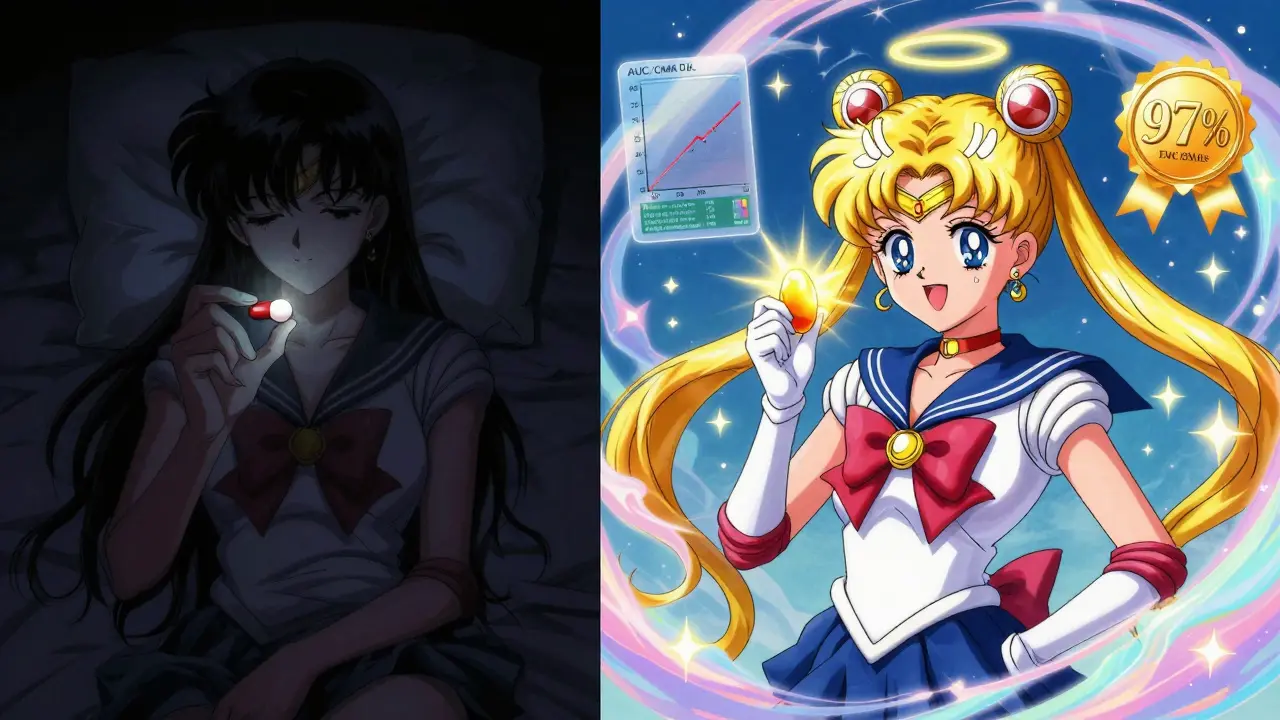
Another layer: complex formulations. Inhalers, topical creams, and injectables are harder to replicate exactly. The FDA has flagged these as higher-risk categories, and only about 3% of generics carry a ‘B’ rating - meaning they’re not considered therapeutically equivalent. For those, you need to pay attention. But for the other 97%? The data says you can prescribe with confidence.
Real-world savings aren’t theoretical - they’re life-changing
Let’s talk numbers. In 2021 alone, generic drugs saved the U.S. healthcare system $377 billion. Since 2009, that total exceeds $2.2 trillion. For a patient on monthly metformin, switching from brand to generic might mean paying $4 instead of $45. That’s not a minor difference - it’s the difference between adherence and abandonment.A 2020 study tracking 3.5 million Medicare beneficiaries found unadjusted survival rates were higher for generic users. But when researchers adjusted for health status - because healthier people are more likely to get generics - the gap closed. That’s critical. It means generics don’t make people live longer. But they make it possible for more people to stay on their meds. And that’s what actually saves lives.
What the evidence says about switching
Many providers worry about switching patients from brand to generic. Will they relapse? Will their blood pressure spike? Will their seizures return?The FDA’s own switch-back analysis found no increase in patients returning to brand-name drugs after starting a generic. Across 12 different medications, the rate of switching back was unchanged - and statistically insignificant (p=0.37). That’s not just a small difference. It’s proof that, for most patients, the switch is seamless.
Even for transplant patients on tacrolimus - a drug where tiny changes in blood levels can mean rejection - a 2020 study in Nature Scientific Reports followed 84 patients over 42 days, switching them between brand and generic versions multiple times. No clinically meaningful differences in drug levels or rejection rates emerged.

What you should do - and what you shouldn’t
Here’s the bottom line: for 97% of prescriptions, generics are not just cheaper - they’re clinically equivalent. You don’t need to second-guess every switch. But you do need to be intentional.- Don’t assume all generics are the same. Check the FDA’s Orange Book. Look for ‘A’ ratings. Avoid ‘B’-rated products unless you have a clear reason.
- Do educate patients. Tell them the FDA requires generics to meet the same standards. Show them the data. Ask them if they’ve had issues before - and listen.
- Don’t ignore patient concerns. If someone says, “I feel different,” don’t dismiss it. Explore whether it’s the pill, the cost, the stress, or something else.
- Do consider authorized generics. They’re made by the brand company and often have fewer patient complaints, even though they’re chemically identical to other generics.
- Don’t avoid generics for psychiatric or chronic disease drugs because of fear. The data doesn’t support it.
The bigger picture: generics are part of better care
The real question isn’t whether generics work. It’s whether we’re using them to their full potential. In New Zealand, Australia, and the UK, generics dominate prescriptions - and outcomes are strong. In the U.S., 90% of prescriptions are filled with generics. That’s progress. But too many providers still hesitate.When a patient can’t afford their med, it’s not just a financial problem - it’s a clinical one. High blood pressure doesn’t care if the pill is blue or white. Diabetes doesn’t care if it’s branded or generic. What matters is whether the patient takes it.
Generics aren’t a compromise. They’re the standard. And the data doesn’t just support their use - it demands it. If you’re still prescribing brand-name drugs when a generic is available, ask yourself: is it because of science? Or because of habit?
Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generics to prove they deliver the same active ingredient at the same rate and amount as the brand-name version. Large studies involving over a million patients show no meaningful difference in outcomes for cardiovascular, diabetes, and most neurological drugs. For 97% of generics, the FDA rates them as ‘therapeutically equivalent’ (A-rated).
Why do some patients say they feel worse on generics?
Often, it’s not the drug - it’s the change. Generics can look different: different color, shape, or size. Patients may associate that with lower quality. Some studies show higher rates of perceived side effects or discontinuation when patients are switched without explanation. Even authorized generics (made by the original brand) show similar patterns, suggesting it’s psychological, not pharmacological.
Are there any drugs where generics aren’t safe to use?
Rarely. About 3% of generic drugs are rated ‘B’ by the FDA, meaning they’re not considered therapeutically equivalent. These are usually complex formulations like inhalers, topical creams, or narrow therapeutic index drugs like warfarin or levothyroxine. For these, check the Orange Book and consider sticking with brand-name or authorized generics unless you have strong evidence supporting the switch.
Do generics cause more side effects?
No. FDA data from 2015-2020 shows only 0.02% of all adverse drug reports involved generic-specific concerns. Brand-name drugs accounted for 3.2%. That’s a 160-fold difference. Side effects are tied to the active ingredient - not whether the pill is generic or branded.
Should I always prescribe the cheapest generic?
Not necessarily. While most generics are interchangeable, some patients respond better to one manufacturer’s version than another - especially with complex drugs. If a patient is stable on a specific generic, don’t switch them unless there’s a compelling reason. But don’t default to brand-name just because a patient is used to it. Ask: Is this helping? Or just familiar?

Monica Slypig
February 2, 2026 AT 17:36Let me get this straight - we’re trusting some generic pill made in a factory in India with no oversight to replace my $45 brand-name med? The FDA? Please. I’ve seen the reports. The active ingredient might be the same, but the fillers? The binders? The coating? That’s where the magic (or the disaster) happens. My cousin’s BP spiked after switching - guess what? The generic had a different dye. They don’t test that. They don’t care. And now they want us to believe this is science?
Becky M.
February 3, 2026 AT 09:15I get why people are nervous - I used to be too. But after working in community pharmacy for 12 years, I’ve seen the real story. Most patients who say they ‘feel different’ are just startled by a new pill shape. I always take 30 seconds to say: ‘Hey, this is the same medicine, just cheaper. The FDA checks it twice as hard as the brand.’ And guess what? 9 out of 10 patients stop complaining within a week. It’s not the drug. It’s the fear. And we can fix that with a little kindness and clarity.
jay patel
February 4, 2026 AT 01:40Look, I come from a country where generics are the only option for 90% of people - and we don’t have a choice. But here’s the thing: even in rural Bihar, where people have never seen a brand-name drug, outcomes are fine. Why? Because the medicine works. The problem isn’t the generic. The problem is the narrative. We’ve been sold this idea that expensive = better. That’s marketing, not medicine. And now we’re stuck with a culture where patients panic because their pill turned from blue to white. The science is clear. The fear is manufactured. Let’s stop letting corporations profit off our anxiety.
Ansley Mayson
February 4, 2026 AT 20:1497% A-rated? Cool. So what’s the other 3%? The ones that kill people. You think that’s acceptable? You think it’s fine to gamble with someone’s life because it saves $40 a month? The data says ‘mostly fine.’ That’s not good enough. One bad outcome is one too many. And don’t give me the ‘it’s perception’ line - perception becomes reality when someone ends up in the ER.
Hannah Gliane
February 6, 2026 AT 15:02Ohhh so now we’re supposed to trust the FDA? 😂😂😂 The same agency that let opioids flood the country? The same ones who approved Vioxx? The same people who approved the first COVID tests that didn’t work? 🤦♀️ You want me to trust a pill that looks like a M&M because some spreadsheet says it’s ‘bioequivalent’? I’ll stick with my brand-name, thanks. My life isn’t a cost-benefit analysis for some insurance CEO.
Murarikar Satishwar
February 6, 2026 AT 20:43Let me offer a different perspective. I’ve worked with patients in both India and the U.S. - and the truth is, the drug doesn’t care where it’s made. What matters is consistency. If a patient is stable on a specific generic, don’t switch. But don’t assume brand-name is better. The data is overwhelming: for most drugs, outcomes are identical. The real issue isn’t the pill - it’s communication. If you explain why you’re switching, if you listen when they say they feel off, and if you give them time to adjust - the success rate jumps to 95%. It’s not about the generic. It’s about the doctor-patient relationship.
Ellie Norris
February 8, 2026 AT 05:50Just had a patient come in yesterday crying because her insurance forced her off her brand-name antidepressant. She said she felt ‘numb’ and ‘dull.’ We switched her to the authorized generic - same manufacturer, same pill, just cheaper. She’s been fine for 3 weeks. The difference? She knew it was the same company. That’s the key. It’s not the chemistry. It’s the trust. And we’re the ones who hold that trust.
Marc Durocher
February 9, 2026 AT 14:03Bro, I used to be the guy who always prescribed brand-name. Until I saw my mom on $4 metformin instead of $50. She didn’t die. She didn’t crash. She just… kept taking it. That’s the whole point. The brand-name isn’t better. It’s just more expensive. And the people who can’t afford it? They stop. And then they end up in the hospital. That’s not science. That’s negligence dressed up as caution.
clarissa sulio
February 9, 2026 AT 22:23Generics are fine. I’m not scared. But if my doctor wants to switch me, he better tell me why - and not just because the insurance company told him to. I’m not a number. I’m a person. And I deserve to know what’s in my body.